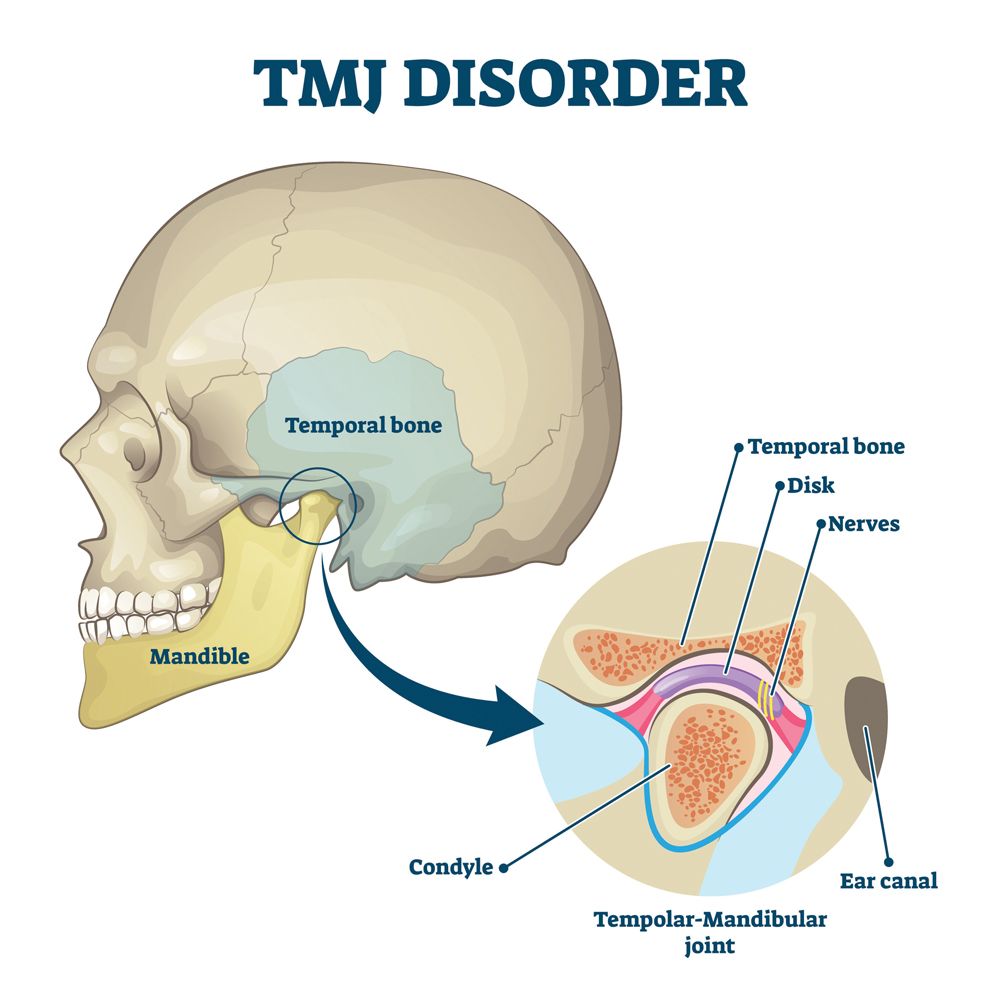
To have proper treatment, there must be an accurate diagnosis. It is, therefore, bewildering to observe consistent efforts to address the condition known as temporomandibular joint dysfunction (TMJ) and only assume that the original attention to the condition arose from the clicking sound from the joint, leading to the supposition that the joint was the origin of the condition, which is incorrect.
When observing the cephalometric x-ray of a patient, dentists are generally interested in the skeletal relationships of the mandible to the maxilla and less to the skull. Because many dentists are not aware that the skeletal relation depends on the maxilla always being in the same relation to the skull (which it is not), the Andrews dental and skeletal classifications are not the same and have major implications in treatment.
During a child’s growth and development, the tongue is responsible for the normal growth of the maxilla, both laterally and anteriorly. The normal position of the tongue is just behind the upper incisors within the bony arches. As the tongue increases in size, it puts pressure on the bony arches, which respond with growth, continuing until the expansive force of the tongue is equaled and contained by the facial musculature.1 Should there be factors that make it difficult for the individual to breathe normally in this manner, the mouth is opened to facilitate breathing and the impetus for growth of the maxilla is lost, resulting in a maxilla that is shorter and narrower than it should be. This results in maintaining the mandible in a retruded position in respect to the base of the skull (the temporomandibular relation), and forward head posture results with a diagnostic loss of the normal cervical lordosis. This is readily viewed on the cephalometric x-ray, and the normal lordosis is regained when the mandible is advanced to its proper relationship to the skull.2 The mouth breathing also has been implicated in suppressing the eruption of the posterior mandibular dentition, increasing the overbite.3
GrindRelief PRO
GrindRelief PRO does not require models, laboratory fees, or multiple appointments. With this new bruxism treatment, you can offer economical therapy the same day you diagnose. Invented and patented by a dentist who suffered from bruxism, the appliance features a unique Central Power Bar, to prevent bite-through and reduce harmful muscle activity by 60% or more.
Grind Guard Technologies, LLC
877-401-1224 | grindreliefpro.com
Should this condition go unrecognized and untreated during the early years, attempts to treat an adult by simple mandibular advancement are likely to be unsuccessful as the maxilla would be situated short of where it should be skeletally. Thus, a Class I restoration would still have mandibular retrusion to some degree.4 Early warning signs include cross-bite, Class II dental, snoring, and medical histories of asthma or allergies, as well as lesser ones such as thumb sucking.
LightWalker Lasers
NightLase is a dual-wavelength laser system by Fotona. NightLase snoring and apnea treatment results in improved nasal breathing and reduces the effects of sleep apnea by decreasing the amplitude of snoring by means of a gentle, laser-induced tightening effect caused by the contraction of collagen in the oral mucosa tissue.
Fotona
888-550-4113 | fotona.com
The Vivos mmRNA Device
The Vivos System from Vivos Therapeutics, Inc, is an advanced multidisciplinary therapeutic protocol for treating mild to moderate OSA, snoring, and sleep-disordered breathing in adults. Offering an all-natural, nonsurgical, and pain-free approach, the system combines the use of oral appliance technology prescribed by specially trained independent dentists with cooperation from their medical colleagues.
Vivos Therapeutics
866-908-4867 | vivoslife.com
If lateral expansion is required to accommodate all of the dentition, the expansion should be done with an appliance such as a Schwarz appliance, rather than a rapid palatal expander (RPE), since it has been reported that an RPE can produce buccal resorption of the roots of the teeth being moved.5 Extraction should be avoided because that shortens the maxilla and closes down the bite, both of which distallize the condyle. During treatment, overbite should be eliminated. Although there are clinicians who state that the mandible rotates around a point in the condyle, this is not true. This can be readily seen by superimposing 2 cephs of a patient with a deep bite: 1 closed and the other opened to the point where the occlusal planes of the 2 arches are at the same level. This, then, allows the clinician to advance the mandible bodily to its proper relation to the base of the skull (and with the maxilla, if it is in its proper relation to the skull). For those who would worry that the condyle is further forward than they were taught, the condyle will always return to a physiologically correct position where the pull from the retrodiscal lamina is equal to that from the lateral pterygoid.6 This is why little can be done to reposition the disc, whereas mandibular repositioning is effective in disc reduction. Failure to reduce the disc is the probable cause of the tension headache.7
In advancing the mandible, I find that using a mandibular appliance is more efficient, more easily tolerated, and less conspicuous, as it is going to be used 24 hours per day (except for brushing, etc). Some would advocate surgical advancement of the mandible as a preferable treatment option. Although there are some studies that maintain good esthetic results, they fail to examine the effect on the joints. The study by Schelhaus et al does examine the joints and reflects an almost universal failure.8 This is because the procedure does not advance the mandible but lengthens it in order to line up teeth. Only the anterior segment (the tooth bearing segment) is advanced. The retrusion and disc displacement, if they exist, persist with its sequelae.
While reading some of the articles on obstructive sleep apnea and sleep patients, I notice that the authors frequently mention that the patients, in addition to the sleep problem, have TMJ. One can only wonder how much of a benefit to the patient it would be to correct the retrusion.
References
1. Santander H, Zúñiga C, Miralles R, et al. The effect of a mandibular advancement appliance on cervical lordosis in patients with TMD and cervical pain. Cranio. 2014;32(4):275-281. doi:10.1179/0886963414Z.00000000038
2. Brodie AG. Muscular factors in the diagnosis and treatment of malocclusions. Angle Orthod. 1953;3(2):71-77.
3. Cooper BC. Nasorespiratory function and orofacial development otolaryngologic clinics of North America. Otolaryngol Clin North Am. 1989;22(2):413-441.
4. McNamara Analysis. The Functional Orthodontist July/August 1992.
5. Barber AF, Sims MR. Rapid maxillary expansion and external root resorption in man: a scanning electron microscope study. Am J Orthod. 1981;79(6):630-652. doi:10.1016/0002-9416(81)90356-0
6. Harris HL. Effect of loss of vertical dimension on anatomic structures of the head and neck. JADA and The Dental Cosmos. 1938;80(2):175-193. doi:10.14219/jada.archive.1938.0030
7. Isberg A, Widmalm SE, Ivarsson R. Clinical, radiographic, and electromyographic study of patients with internal derangement of the temporomandibular joint. Am J Orthod. 1985;88(6):453-460. doi:10.1016/s0002-9416(85)80044-0
8. Schelhaus KP, Piper MA, Bessette RW, Wilkes CH. Mandibular retrusion, temporomandibular joint derangement and orthognathic surgery planning. Plast Reconstr Surg. 1992;90(2):218-229.