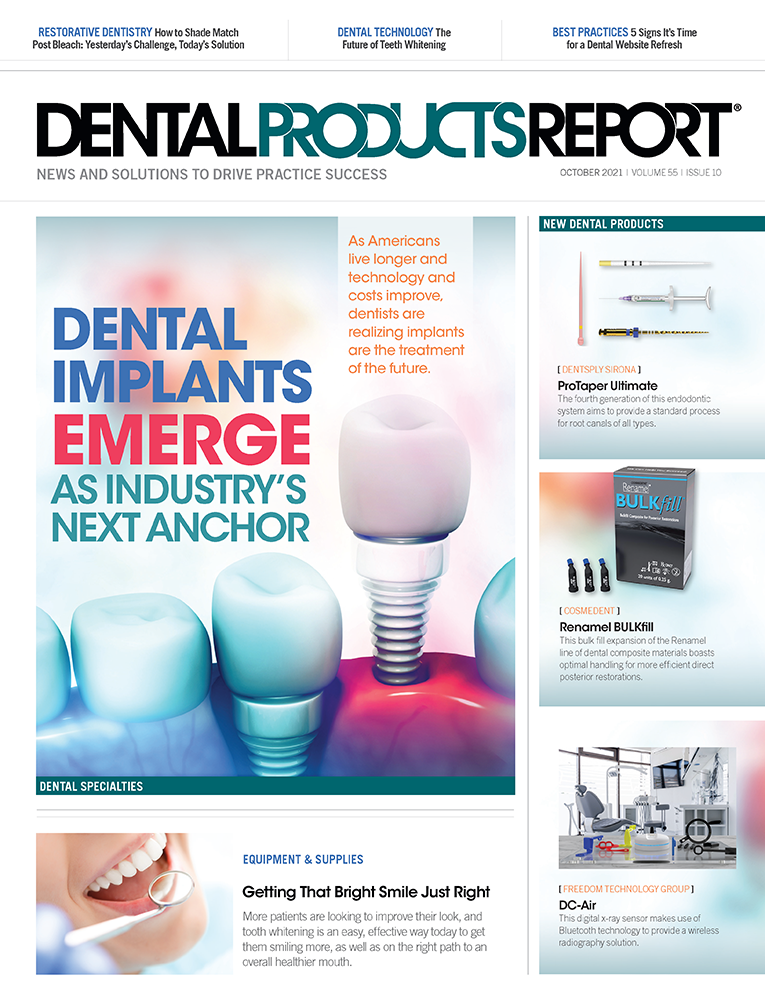
Dental Implants Emerge as Industry’s Next Anchor
As Americans live longer and technology and costs improve, dentists are realizing implants are the treatment of the future.
Dental Implants Emerge as Industry's Next Anchor. Photo courtesy of Crystal Light / stock.adobe.com

As many as 120 million individuals in the US are missing at least 1 tooth, according to the American College of Prosthodontists. And 36 million Americans have no teeth at all.1 If one of these patients is sitting in your chair, how would you replace their teeth? For many clinicians, the answer is dental implants.
Many clinicians consider dental implants to be the standard of care for replacing missing teeth. Dental implants often lead to successful and long-lasting restorations. A recent study published in the International Journal of Prosthodontics suggests that implants supporting a single crown or a partial denture had a survival rate as high as 92% at 12 years.2
Sundeep Rawal, DMD, a Florida prosthodontist, cofounder of the Digital Dentistry Institute, and senior vice president of implant support at Aspen Dental Management, says that success gives patients the optimal outcome for restoring teeth functionality.
Alexander Shor, DMD, MSD, and Jim Janakievski, DDS, MSD, founders of 35Newtons, agree that implants are the best alternatives for tooth replacement because they act like natural teeth.
“People are living longer,” Dr Janakievski says, “but their teeth are not lasting as long. As specialists, it surprises us that we have older patients wanting more complex treatments. Years ago, we would have patients in their 90s refuse implants, but now they routinely request implant treatment.”
With patients living longer, “we have to design our implant treatment to be retrievable,” Dr Shor says. “This means implant position and abutment design that allow for screen channel access.”
N. Cory Glenn, DDS, AAID, clinical director of technology for dental implant company Blue Sky Bio and a partner in Transcend Dental Education, says the increased awareness of dental implants’ long-term restorative performance has boosted their prevalence as a treatment option.
“The biggest reason we’re seeing such huge growth in the implant industry right now is that everybody has wised up,” Dr Glenn says.
“Oral health and oral esthetics have become increasingly more important for dental consumers,” Craig Hennings, president of SICAT USA, says. “From a patient perspective, they don’t view it as an implant as much as they view it as a tooth replacement.”
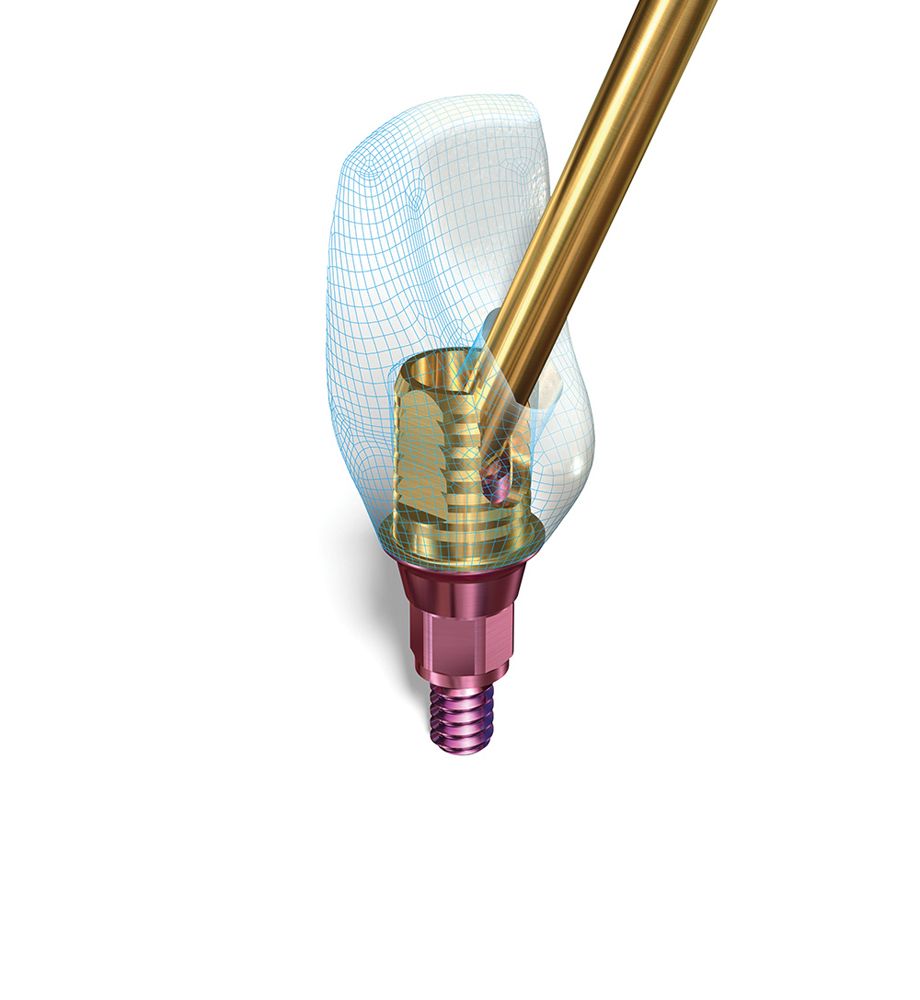
FirstPlug from 35Newtons is an abutment screw barrier. Using this, clinicians can ensure proper connection between the implant and the abutment. Combining advanced, accessible technology with the proper tool has made implants and other restorative treatments something that any modern practice can boast.

Generational changes also reflect a changing consumer attitude toward implants, Hennings says. For example, many baby boomers (those born between 1946 and 1964) who have had ongoing issues with failed bridges or root canals now see implants as a viable option. At the same time, Generation X (those born between 1965 and 1980) and millennials (those born between 1981 and 1996) consider oral health a critical part of their overall health.
“With the baby boomers and their access to that kind of dental care combined with the upcoming generations that view dentistry more favorably, it portends to a viable long-term solution that implant placement as a discipline within the practice is going to be highly sustainable,” Hennings says.
However, the increase in dental implants isn’t just patients’ changing attitudes. Dentists’ perceptions have changed, too.
Wayne Harrison, DDS, vice president of operations and clinical affairs for Ditron Dental and a fellow of the Academy of Osseointegration, says to compete with large group practices and dental service organizations (DSOs), dentists will have to incorporate all kinds of specialty treatments, including dental implants.
“To sustain themselves in the marketplace, they’re going to have to be super dentists,” Dr Harrison says. “They’re going to have to learn to do other things and incorporate implants into their practice where otherwise they may have [stayed] away from that just to be able to compete with the DSOs that have everything in-house.”
In addition to changing attitudes, changing materials, technology, and technique contribute to the trend. Matthew R. Young, DDS, a diplomate in implant dentistry of the American Board of Oral Implantology (ABOI) and a fellow of the American Academy of Implant Dentistry (AAID), says new implant surface technology has improved bone-to-implant contact.
Also, advances in digital dentistry provide a predictable implant restoration with a better fit and precision than traditional workflows. In addition, the procedures are more comfortable for patients and today’s protocols improve recovery time, allowing for immediate temporaries to restore function the same day.
“Dentists want their patients to be back in action and functioning properly. The goal is to have minimal interruption of our lives. These are all wins,” Dr Young says.
The Anatotemp SC healing abutment and scan body, a recent addition to exocad’s and 3Shape’s dental implant laboratory and model creator software, offers a streamlined digital workflow.

“There are now better surfaces. There are also faster treatment concepts,” Pascal Kunz, MD, DDS, vice president of digital solutions for Envista and its DTX Studio Suite software, says. “Something that took 6 months to a year until a final restoration outcome [now] can be done in the same day to the provisional and much earlier to the permanent restoration.”
In addition to the surgical benefits, Felix Chung, CEO of Imagine USA, says technology also improves prosthetics on the restorative side. The dramatic and geometric shape of dental implants necessitates precision in both engineering and manufacturing. Imagine USA improves the technology to cater to the increase in demand for implants that require a high level of precision, a trend that Chung sees throughout dentistry.
The patient is there for the prosthetic, which technology helps dentists visualize instantly and effortlessly, Dr Kunz says. Technology for implant placement has produced surgical guides and even dynamic 3D navigation with products such as X-Guide™, which can provide turn-by-turn guidance to improve precision and accuracy of implant position, angle, and depth.
“So now you know exactly what you could do and what you should do, and you have the technology to help you do it,” Dr Kunz says. “We are now at the stage where technology is helping you, not making things more complicated.”
“Using digital technology for implants is going to accelerate the shift to the treatment with the digital technology we see in dentistry,” Chung agrees.
Louis Vodopivec, director of product strategy for Planmeca USA, recognizes that another vital driving force behind implants’ growth in dentistry is the value patients place on their teeth and smile combined with increased access to the financial means to afford them.
“When you combine that with the rise of social media and the current standards of beauty and seeing ourselves on video conference calls, it’s difficult to not get caught up in this unique era that we live in that increases the natural demand for esthetic dental solutions. Along with orthodontics and clear aligners, tooth whitening, veneers, and modern composite restorations, implants are a key tool for overall patient health care, esthetics, and the outcomes that patients want to experience,” Vodopivec says.
Dr Harrison, who was the previous training and education manager for Nobel Biocare, says education will drive the future of implant dentistry. When dental school programs teach implants, more dentists see opportunities to place implants.
“When I was lecturing for Nobel, I used to say, ‘Do we only see what we know, or do we only see what we have a solution for?’ Many dentists never saw a dental implant because they did not understand them. The only solution they had was a bridge or a partial denture. That’s still very apropos today,” Dr Harrison says. “So as education moves from the hotel room to the classroom, that is going to drive the industry further.”
“This is the future,” Robert Martino, DDS, CEO of Wilmar Management and OraCare, says. “I don’t think we are going to be doing fewer implants.”
Realizing This Future Might Require Some Help
Dental implants have come a long way since the first placement in the 1960s. However, dental implants still have obstacles to overcome.
Liz Lundry, RDH, clinical education manager for StellaLife, says one of the most significant obstacles is clinicians not presenting implants in the treatment plan.
“If we know that [patients] may be going through difficulty in their life, like a loss of a job or a divorce or an illness or...financial issues, a lot of times we won’t present things to them. When we do that, we are making the decisions for them and discriminating against patients. It’s not fair to patients,” Lundry says.
Fabricated from 8 components including materials from a range of sources and workflows focused on quality and detail, Alien 8 restorations from Alien Milling are lightweight implant-supported full-arch solutions that reportedly offer both esthetics and flexible strength.

Another obstacle is cost. Hennings says the lack of widespread insurance coverage for implants puts the treatment into an elective category, even though it may be better than treatments insurance covers.
“Unfortunately, consumers often times default back to what is covered,” Hennings says.
Dr Rawal says overcoming that financial barrier is essential.
“We know what we can do with dental implants impacts so much of the patient’s life from their oral health to their overall systemic health, their confidence, lifestyle, and self-esteem to their psychological and emotional health,” Dr Rawal says. “You can justify that the therapy is worth the investment.”
However, Dr Rawal says the most significant obstacle for dental implants’ future is clinician confidence in their ability to place them.
Without exposure to dental implants and full mouth restorations in dental school, dentists lack the knowledge, skill, and expertise that contributes to that confidence.
“That’s one of the main reasons at Aspen we emphasize training for our doctors, to allow them to learn, excel, and gain confidence with offering important services to patients,” Dr Rawal says. “If we can offer implant therapy and do it in predictable, innovative ways that we have today in dentistry, the results speak for themselves.”
Access also has been an obstacle for dental implant therapy, Vodopivec says. Many patients do not follow through with the referral to a specialist. Vodopivec says that as more general practitioners recommend implants to their patients, more patients will get them.
“The majority of dentists should be cherry-picking the best straightforward cases and providing that service in the general dentist’s office and referring more of the complex cases to a specialist,” Vodopivec says.



A patient receives implant treatment using FirstPlug Abutment Screw Barrier from 35Newtons. Founder of 35Newtons Alexander Shor, DMD, MSD, and Jim Janakievski, DDS, MSD, both agree that implant treatment is a useful and powerful restorative tool. They both emphasize the importance of becoming familiar and mastering any new implant system instituted at the practice. There also has been a noticeable uptick of older patients coming and receiving implant treatment. To Drs Shor and Janakievski, this means having implant position and abutment design that allow for screen channel access. This is why they began 35Newtons, to ensure that they would have a customizable abutment experience that would work for patients in all age groups with the need for any kind of implant treatment.

The learning curve for dental implants can be an obstacle, too. Dr Glenn says the critical thing to understand is implants are not just surgical or prosthetics—they are both. Moreover, the patient doesn’t want an implant; a patient wants teeth.
“They don’t care about the surface treatment or the technical connection or whatever else,” Dr Glenn says. “Patients want their teeth back. So our job is to get them to that point.”
Implant companies also have obstacles, Chung says. For example, some new implant companies and even some traditional ones don’t have a digital component, he explains. However, within 5 years, the next step will be to scan in almost every type of implant placed, he says. That means the entire implant treatment planning, surgical, and restorative process will be digital from start to finish.
“It’s crucial as companies start to grow [that] they invest heavily on different components that work with digital technology,” Chung says. “Those companies that have are going in the right direction.”
Moving Forward
Going in the right direction with implants requires addressing challenges and overcoming these obstacles, starting with confidence and experience.
Dr Rawal says clinicians should incorporate implant dentistry early in their career and keep learning as techniques and technology improve.
“It’s important that not only do we ensure our clinicians can provide optimal dental implant therapy today as part of their practices, but also that they’re learning the skills, techniques, technologies, and innovations that allow them to offer those therapies in the most innovative ways possible,” Dr Rawal says.
“Dental school does a great job, but it’s not real-world dentistry. So when you get out of there, you have to learn things,” Dr Martino says.
Dr Martino runs a mini-DSO for 7 practices in West Virginia. He thinks all doctors should know how to place implants, or at least know how to restore them. So his dentists acclimate to real-world dentistry after school and then attend training where implants are part of the curriculum.
“If they are interested, once they get their feet under them, we get them more training,” Dr Martino explains.
“I feel training is paramount for dentists,” Hennings says, adding that SICAT USA has a wide variety of local and national education options for training with their key opinion leader partners.
SMARTbase abutments from Implant Direct are designed with dual hue anodization to seamlessly blend with surrounding dentition. With a variety of cuff heights and widths available, the abutments can be used with a range of situations.
Dr Young recommends the resources at the AAID, where he is an executive committee board member. AAID sponsors credentials in implant dentistry and Maxicourses™ with 300 hours of hands-on courses. These Maxicourses teach biology, dental implant theory, clinical approach to surgical and restorative phases, implant surface textures, guided surgery, and 3D-planning surgical techniques, among other subjects.
“Both the AAID and the ABOI are organizations [that] want our colleagues to succeed,” Dr Young says. “But in the end, the most important part is [that] it helps with patient care.”
“The Kois Center and Spear Education and those kinds of mentors also offer postgraduate courses without having you do a 3-year program. So that offers a lot of opportunities for dentists to go to the next level,” Dr Harrison says.
Dr Glenn thinks guided surgery is a game-changer for decreasing the learning curve. It helped him have an ideal restoration in mind from the start.
In the past, surgical guides for dental implants were extremely expensive, Dr Glenn says. However, Blue Sky offers a guided surgery plan starting at $11 for the export. Also, some dentists think making a surgical guide is a complex process that requires a laboratory, but Dr Glenn says that isn’t true.
“Maybe that was the case 5 years ago. It is not the case for how we are routinely teaching people to do this today,” Dr Glenn says.
SICAT software starts with the end in mind. Hennings says clinicians can use the SICAT software to determine the optimal angulation and depth virtually.
A proficient dentist can have a treatment plan in front of the patient in a matter of minutes, from angulation and depth, and even put a digital restoration on top of that so the patient can see how it will look.
Vodopivec agrees, adding that a full suite, such as Planmeca’s Romexis software, is essential for planning and creating surgical guides.
The NeossONE™ prosthetic platform from Neoss is suitable across 3 implant ranges—1 impression coping, 1 implant replica, and 1 abutment interface.The NeossONE platform uses a minimum number of components and can be used for long-term performance.

“You can plan the implant placement right in front of the patient. You can show them exactly where you want it to go and how much bone they have. The patient can understand the case,” Vodopivec says. “From there, you can also design a surgical guide within the same software and send that surgical guide to a 3D printer or a milling unit.”
Technology also reduces the costs throughout the restorative part of the implant process. In the past, dentists could expect a 2-week turnaround and a $500 bill for a custom abutment and crown. However, Dr Glenn uses the Versamill 5X400 from Axsys Dental Solutions to handle it in-house, reducing their costs to a $50 titanium abutment blank and a zirconia block.
“The savings get even bigger when you start thinking about full-arch restorations. A zirconia hybrid would usually run around $4000 from a lab, whereas we can get 2 full arch hybrids out of a single $100 zirconia puck. Also, for our full-arch surgeries, we’re often skipping the process of doing a traditional denture conversion, which is stressful and time-consuming. Instead, we can scan at the time of surgery and design and mill a perfect full-arch hybrid in PMMA the same day for $30, and it will be far stronger,” Dr Glenn says. “Bottom line, having the Axsys scanners and mills opens up a world of possibilities for us that dramatically reduces our overhead and gives us faster and better results.”
Dr Young recommends investing in CT technology. CT scans give clinicians a 3D evaluation of bone. Merging a digitized version of the patient’s teeth with a CT scan allows dentists to plan where to place the implant in the best available bone in the safest position.
Preplanning allows experienced dentists to decrease the surgical time. However, the technology also benefits dentists inexperienced in placing implants. It lets them become familiar with the patient’s jaw before they start and gives them a solid protocol for the placement.
“It dramatically decreases the learning curve,” Dr Young says.
Vodopivec says it’s essential for GPs to have the 3D image and the software platform to plan and execute the surgical guide in-office. It is also critical to partner with a manufacturer who provides training.
“With Planmeca, you get cone beam computer tomography [CBCT] training as well as basic implant training, and from there, it’s an easy path through additional courses through educational institutions to continue implantology,” Vodopivec explains.
Other CT companies offer access to a radiologist when you buy their equipment. For example, KaVo Imaging has partnered with BeamReaders to offer GPs 60 radiology reports in the first 60 days of ownership of an OP 3D or i-CAT FLX to help them as they learn about CBCT.
Embracing a digital workflow is also essential to decreasing the learning curve. Chung says it is imperative that dentists placing implants use digital technology and invest in an intraoral scanner.
“The most accurate way to make an implant prosthetic on top of your implant is to scan it. If they go the traditional impression route, they are not going to get the most out of the current materials or technology,” Chung says.
Maintaining the prosthetic is also essential. OraCare developed the REASSURE implant care kit to help address the biofilm issue that leads to peri-implant diseases that can lead to implant failure. Chlorine dioxide is the main ingredient, and the system begins with a gel the dentist uses right after the placement to control bacteria.
After the healing process for the implant completes, the patients use the OraCare rinse twice a day to help prevent biofilm at the implant site.
“We have seen great results, from tissue management to implant site cleanliness,” Dr Martino says.
Reducing pain and inflammation also leads to better outcomes. Lundry says that StellaLife products accelerate healing and reduce pain. Results from StellaLife studies at the University of Bern and University of Texas indicate that StellaLife VEGA oral care rinse accelerates healing by stimulating growth of fibroblasts.3,4
“Our products can help tremendously in cases of peri-implantitis,” Lundry says. “All StellaLife products reduce pain and inflammation for better clinical outcomes.”
35Newtons is addressing challenges in implant restoration workflow. For example, there was no specific material designed for management of the screw channel, so dentists improvised, using plumber’s tape from the hardware store. The polytetrafluoroethylene (PTFE) material is stable and hydrophobic and it doesn’t degrade, so it’s ideal for the screw access channel. However, industrial manufacturers didn’t intend for it to go in teeth.
Drs Shor and Janakievski optimized a medical-grade PTFE material for their FirstPlug® Screw Channel Barrier, making it a better size, easier to place, and more packable than plumber’s tape. It is the same medical-grade material used for vascular stents, sutures, and membranes, and it is FDA registered.
“Those products are manufactured under strict guidelines for use in the human body,” Dr Janakievski says. “We felt it would be important to have it manufactured under those standards.”
Re-treatment
Planning for future retreatment of a case is critical.
“Another principle would be to try to design everything in the way that it can be re-treated later, removed easily from a patient’s mouth for maintenance,” Dr Shor says.
Dr Janakievski recommends getting trained in the implant system every time a practictioner changes manufacturers.
“Because there are many systems available, it’s very important to learn the details of that system and the need to follow their specific protocols,” Dr Janakievski says.
Dr Kunz suggests that dentists do not look for the least expensive implant system and software or try to put components together on their own. Instead, he advises them to look for solutions from companies with a long track record of success, then learn their program and system. Dr Kunz says finding a mentor and asking them to assist a couple of cases can help clinicians feel more confident in their implant skills. Finally, he recommends careful case selection in the beginning.
“Do not look for the perfect case; look for a straightforward case,” Dr Kunz says. “If you know everything and you prepare adequately, you make it easier and workable. But there are also clearly very complex things to stay away from. You never go to Mount Everest on your first hiking trip.”
If a patient refuses implants, Lundry advises dentists to find out why and address their concern. Lundry says the benefits of dental implants necessitate this persistent approach.
Lundry also wants clinicians to have courage and compassion. By positioning the treatment plan from an area of concern for the patient’s health and well-being and understanding the challenges from the patient’s perspective, clinicians can get patients the treatment they need.
“And if we don’t have the courage, we can use the compassion to build that courage and put it out there for the patient,” Lundry says.
Dr Kunz says a focus on knowledge, experience, and excellence is essential to enjoy the benefits of the dental implant future. It’s important, he says, to put in the time to understand implant dentistry, moving forward with the industry as it improves techniques and technology, and planning with software such as Envista’s DTX Studio Suite.
“It will keep you out of trouble and help you deliver success much more predictably,” Dr Kunz says. “And then it’s a joy and you want to do more.”