Special Report: New Frontiers of Dental Implants
Here is a look at key areas where companies have focused their research, from implant planning automation and implant surface technology design to what is next for abutments, and even how some companies seek to reshape the implant workflow entirely.
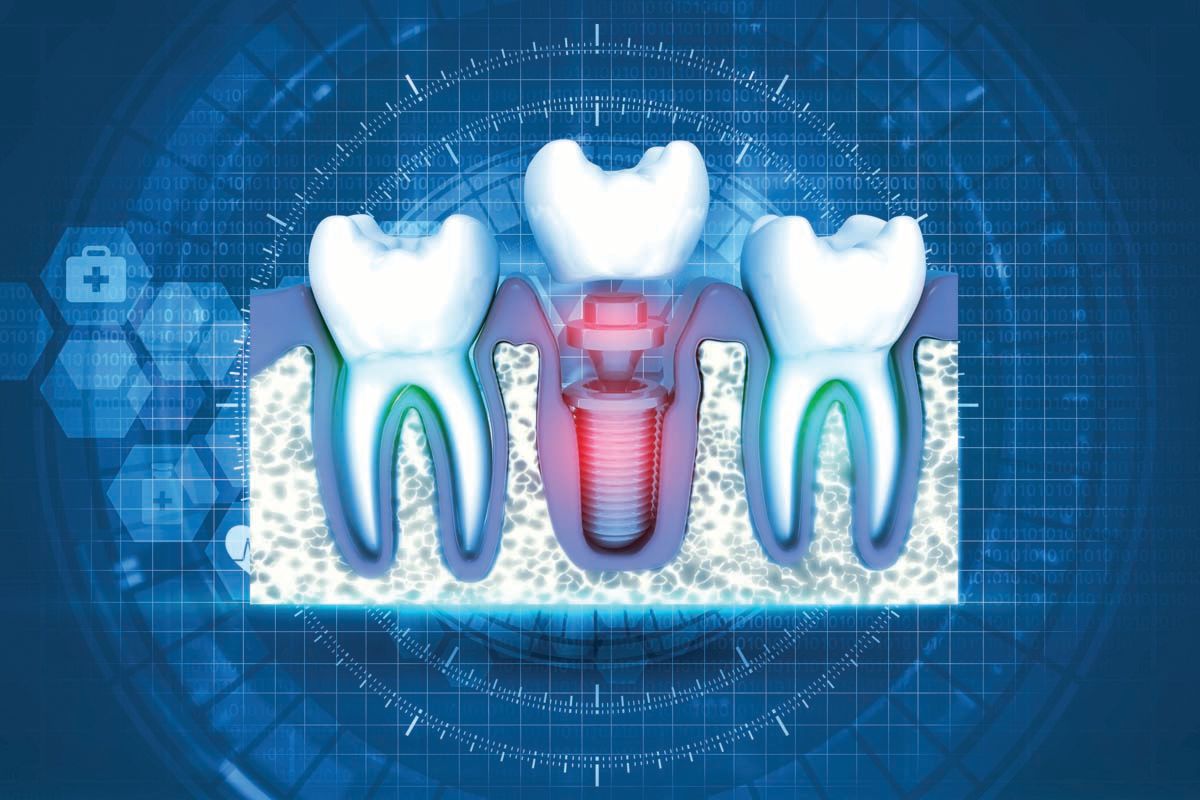
Special Report: New Frontiers of Dental Implants | © Crystal Light -stock.adobe.com
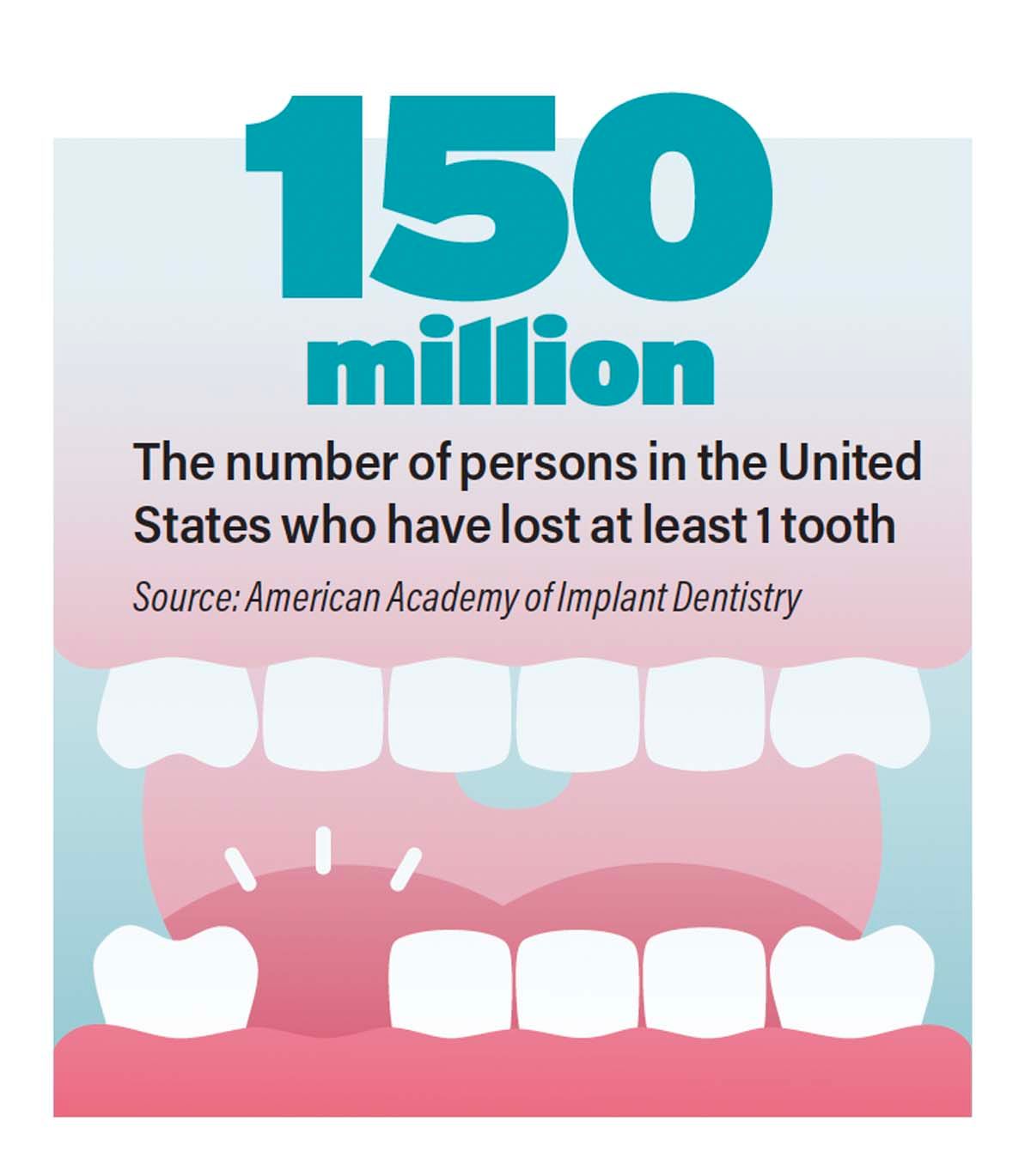
One hundred fifty million—that is the number of persons in the United States who have lost at least 1 tooth, according to the American Academy of Implant Dentistry (AAID). However, clinicians place only 2.5 million dental implants annually.1
That means many individuals are missing teeth. How many of them are your patients?
Adult tooth loss is clearly a fact, at least in the United States. However, implant dentistry is not necessarily the treatment modality these clinicians and patients are choosing today.
However, that could be changing. Some analysts predict growth of the global dental implants market to $9.5 billion by 2032,2 whereas others anticipate steady growth in the United States alone to an estimated $2.2 billion by 2029.3 According to the AAID, the driving factors behind the growth include an aging population, a desire to keep one’s teeth, and growing awareness of the advances in diagnostic and restorative techniques for dental implants.1
So, what advances are piquing these patients’ interest in dental implants?
Implant Planning and Placement: Automation Will Streamline, Workflow
Alon Mozes, CEO and cofounder at Neocis, Inc, says new planning and image diagnostics technologies are an exciting area for today’s implant dentistry. Implant planning is becoming more sophisticated, with more tools at dentists’ disposal. Automation, he says, will support dentists to the point where even those with limited experience placing implants will have more support from software regarding imaging diagnostics and planning for implant placement that takes advantage of bone density in the area.
“The software will be able to highlight if they’re risking damage to any critical anatomy, like the alveolar nerve or sinuses,” Mozes explains. For example, the software for Neocis’ robotic platform The Yomi Robot colorizes the implant’s surface based on the Hounsfield units in the CT scan. He says the system will indicate whether the dentist is planning in excellent or poor bone and will flash red if they are planning too close to the nerve or risking perforation of the sinus. “That makes it much easier for them to think about planning the implant,” Mozes says.
However, planning is only part of the workflow. Implant dentistry is about restoring teeth. To allow more collaboration and communication, Neocis is also developing sophisticated prosthetic planning, allowing dentists to plant the implants and the restorations in 1 central software ecosystem, Mozes explains.
“That enables dentists to plan the complete end-to-end workflow,” Mozes says. “You can restore the patient’s teeth and get the surgical result you want.”
There are different perspectives on the workflow. Some clinicians care most about getting the implant into the excellent bone. However, Mozes says clinicians on the restorative side want to ensure that the emergence axis is precise for easy, functional, and esthetic crown placement. If you place the implant in the bone but the placement is not precise, it can create problems. “When you get to the restorative side where you have to have custom abutments in a much longer restorative process to get the result you’re looking for,” Mozes says, “you can get some very upset restorative dentists, whereas the surgeon may be perfectly content.”
In addition to facilitating collaboration, these enhancements to implant planning also streamline it. Additional support will be available to dentists to outsource their planning and design to Neocis.
“We’ll have support through multiple avenues, whether that’s through the software itself and automated suggestions powered by artificial intelligence or through a planning service we provide as a company to assist the dentists,” he says. “Then it’s very easy to loop in all those stakeholders, the restorative dentist, the oral surgeon or periodontist, and a lab. All of them need to collaborate along this patient journey forthe best result.”
In addition, the robotic platform makes the lab’s job easier. Surgical guides are not necessary. The plan is in the software, and the robot helps the clinician execute it flawlessly. Instead, the focus is on the prosthetic because the robot covers the drilling and placement. Sometimes, the dental practice can use the file to create the prosthetic in-house. “So, that planning software becomes very instrumental in giving the dentists more control over the entire end-to-end workflow,” Mozes says.
The Yomi robotic platform is comprehensive because it allows you to merge your imaging requirements automatically, like a DICOM CT scan and an STL file from the intraoral scanner. Then, the dentist can review the bony anatomy, surface, and soft tissue and precisely plan the implant location and prosthetics preoperatively. However, the platform continues to support the clinician because the robot arm will physically guide the surgeon interactively to ensure they follow the plan exactly, with haptics and visual displays during implant placement.
“The dentist is always in control of the drill, but as they get close to the surgical site [the platform] will kick in if the clinician diverges from the plan and help them adjust. It will show them on the screen in real time as it adjusts and how they’re improving,” Mozes said. “Most importantly, physically, it’s going to feel like it’s easy to move the angle in the right direction, and it’s going to feel very stiff and resistive when they try to move [in] the wrong direction. It doesn’t move by itself. It makes sure you drill exactly where you intended.”
An additional benefit is that with the robot’s guidance, successive drilling will be in the same spot. Performing freehand surgery, Mozes says, can result in an oval-shaped drill hole by minute changes in the angle. Therefore, the implant will have a snug fit because the drill has more precision coming from drilling at the same angle repeatedly. “Implant stability has a lot to do with the life of the implant and the success of how well that integrates,” he adds.
Mozes anticipates automation handling more of the implant planning steps soon. From nerve planning to sinus outlining and even some restorative steps, like sizing and shaping the crown properly, the dentist can have a streamlined process without too much work. Further out, he sees machine learning algorithms, leveraging thousands of cases Neocis has worked on, automating the planning. “At some point,” Mozes says, “you’ll be able just to push a button and say, ‘Tell me where’s the best implant location for this patient,’ or, ‘What is the best restorative solution for this patient?’ and the software will be able to drop in the implant, put a crown on it, and give it to the dentist for a thumbs-up.”
Dental Abutments: Pulsed Electromagnetic Field Provides Novel Treatment for Peri-Implantitis, Faster Osseointegration, and Tighter Soft Tissue Seal
The osseointegration process and healing time are essential considerations in any implant case. Some of today’s implant designs try to address and improve the outcomes in both areas.
Benny Barak, MBA, ADV, CEO of Magdent—founded by Shlomo Barak, DMD, an oral and maxillofacial surgeon, and Moshe Neuman, DMD, a periodontist with an MSc in bone biology—says the hottest topic in implants is understanding how different companies can create a better, tighter seal between the healing abutments and soft tissue to reduce risk of peri-implantitis. The Magdent-MED (miniaturized electromagnetic device) produces a pulsed electromagnetic field (PEMF) proven to accelerate the natural healing process around the dental implant. Barak says Magdent’s PEMF technology could reduce inflammation and change the bacterial biofilm around implants. “With these 2 factors, we were able to create a faster integration and a better and tighter seal between the implants and our healing abutments,” Barak explains.
The FDA cleared PEMF for the use of stimulating bone growthin 1979 and it has been used since then for multiple procedures in orthopedics. Magdent is the first company to use this novel technology in dentistry. The product is undergoing FDA clearance for the US market.
The MED is made of titanium alloy and fits standard healing abutments into the implant. Clinicians need to activate MED before placement in a 5-second procedure; the MED’s battery then generates the PEMF for up to 30 days after activation.
The MED will be compatible with up to 85% of implant brands, with various models available today including most of the internal hex models of Nobel Biocare, Zimmer-Biomet Tapered Screw-Vent, BioHorizons, Camlog, Astra Tech, MIS, Implant Direct, Hiossen, and AlphaBio, among others. A single-use hex driver comes with the MED to seat it and thread it into the implant with only finger pressure.
Doctors working with the MED found that the gingiva was thicker and more keratinized than the soft tissue surrounding other implant sites. However, there are hard tissue benefits as well, as the MED stimulates osseogenesis and osseointegration, Barak explains. A new study Magdent recently published reveals that using the PEMF technology unique to MED allowed clinicians to grow bone for patients with peri-implantitis, which he describes as a game changer.
“We discovered that the MED helps to accelerate bone formation in peri-implantitis cases. With these improvements, the bone held the implant in its location, and they were able to save those implants for those patients,” Barak says, adding that this is also seen in a follow-up study being conducted in Brazil with Jamil Shibli, DDS, PhD, MSc, of Guarulhos University, that is on track to produce the same result.
Other research published by Magdent implies that even patients with poor bone quality—such as those with diabetes, cancer, or osteoporosis, or even heavy smokers—become better candidates for a successful implant placement. The MED’s abutment technology improves success in these cases normally prone to failure.
In addition, the Magdent MED solution is affordable, especially compared with other market options, according to Barak. Some companies with products that reduce bacteria around the implant charge thousands for their solution; Barak says this focuses on only 1 of several aspects the MED addresses. However, with Magdent’s MED, each clinic acquires 1 activator and then MED products for their patients, at an estimated cost of $100 to $120 per MED.
Looking ahead, Barak sees an aging population with a higher emphasis on maintaining oral hygiene, and an increased need for a solution helping high-risk patients, the number of whom has increased due to post–COVID-19 condition. Also, Barak says multiple resources report a growing global competitive annual growth rate for the dental implant industry. The combination of the growing emphasis on oral health and the introduction of more technology will make implants the standard of care. Barak anticipates that Magdent’s patented ability to treat peri-implantitis will only help grow this trend. Magdent MED has had interest from multiple companies across the European market due to Magdent’s CE mark clearance; the MED is expected to soon be available in the US market.
Moreover, the MED is showing excellent results in tripling acceleration of osseointegration and increasing bone quality around the implant. Barak says that in a study Magdent has published that used rabbits, the PEMF technology increased bone-to-implant contact by 48% and bone volume density by 62%.
“These 2 figures, along with the other outcomes that we saw in the study,” Barak says, “really give a dentist the ability to feel more comfortable when they place implants for these patients [who] suffer from poor bone quality because they know that our technology grows stronger bones for their patients while in the recovery stage.”
Implant Design: Balancing Thread Aggression to Aid Immediacy and Control
Indraneel Kanaglekar, senior vice president and global dental president at life sciences firm ZimVie, says that when it comes to implant design, a few trends drive where things are going. First, companies are focused on bone-level implants, not tissue level. In most cases, implants these days are subcrestal, which is driving more innovation in bone-level implants, Kanaglekar says.
The second trend in implant design development is driving toward immediate placement and restoration, which leads to designing aggressive threads that provide instant stability, allowing the clinician to confidently complete the restorationright after placement. However, one of the problems with aggressive threading is that the implant placement can be hard to control, leading to loss of precision, or in some cases bigger complications. This is mainly if the clinician is not precise enough to keep the placement from deviating, Kanaglekar says. Therefore, development is focused on obtaining precision of placement with primary stability.
“The implant design is moving towards being fully tapered with more aggressive threads while still giving sufficient control to the clinician and striking the right balance between control and aggressiveness to provide immediate solutions,” he says. “With our implants, the T3 PRO and TSX, we worked on that balance where you get the right amount of placement torque and bone-to-implant contact ratio, giving confidence to the clinicians of primary stability while ensuring excellent control.”
In addition to striking a balance between aggression and precision of the design, the engineering team at ZimVie also had to ensure the new implants were compatible with the existing instrumentation and surgical set.
“It was about measuring 2 things: the bone-to-implant contact, which gives primary stability, as well as the torque level when you place the implant,” Kanaglekar says. “We ensured that we achieved that while not going overboard regarding how much the threads protrude from the implant body.”
A third trend in implant design is optimizing the roughness of the surface to enhance osseointegration. Kanaglekar says this effort is significant in the coronal portion of the implant to mitigate the risk of peri-implantitis complications that can create bone loss. ZimVie’s new implants have an acid-etched surface on the top, which is rough enough where it is going to allow bone growth but not excessively rough that it causes infection issues. ZimVie’s acid-etching technology creates a surface roughness that is not hospitable to bacteria, creating peaks and valleys that they cannot reside in, Kanaglekar explains.
“Some companies leave the collar completely polished to minimize the chances of bacteria adhering to it, but that also decreases the chance of initial bone growth after you place the implant because it’s so smooth. So, we believe that getting the balance right is important, and we believe that acid-etching surface technology is an optimum surface roughness that allows the best solution,” Kanaglekar says.
ZimVie is addressing implant design in other ways. The new implants handle various indications with differing sizes and lengths. Also, ZimVie is expanding its portfolio with continuous enhancements to digital workflow, ensuring that the implant procedure is simple and efficient in terms of the total time it takes, uses fewer physical materials, and produces more long-term implants.
“It’s a holistic approach,” Kanaglekar says. “You can’t focus just on software. We start with the intraoral scanner’s integration with the software. Then, it’s going to software that can help dentists plan the surgery and design the guide. After the surgery, our proprietary Encode® technology makes the impression procedure very simple. Then we focus on our patient-specific solutions and how to make it as easy and intuitive as possible.”
Looking forward with implant design, he says the goal would be to make the procedure as simple and patient specific as possible. For now, there are far more crowns and bridges than implants today.
“We ultimately want to come to a point where no matter which dentist you go to, they are going to recommend an implant if you have a missing tooth,” Kanaglekar says. “The advancement of technology and improvement in clinical outcomes should eventually lead to implants being the only solution for a missing tooth.”
Implant Design: Patient-Specific Implants Replace Implant Systems
Iris Wedeking, MBA, CEO and cofounder at iDENTICAL™, says implant design is taking digital dentistry to the next level by challenging the idea that the surgery needs a drill. iDENTICAL’s patented technology creates a personalized, 3D-printed titanium implant modeled from the patient’s tooth. The dentist extracts the natural tooth, scans it, and then sends the scan to iDENTICAL. iDENTICAL then uses its patented design features to create a personalized dental implant the dentist inserts into the patient’s native socket site, no drilling required.
Wedeking says there are numerous benefits to this fully digital workflow. First, because the implant is manufactured based on the patient-specific design, it fits in the socket without drilling. Also, the workflow skips the 3- to 6-month healing time because no bone grafting is required. This makes implant dentistry more accessible; you can place these implants with minimal training because no drilling is required. Placing the implant requires a specially designed inserter, after which the clinician gently taps it into place.
Per Wedeking, the 3D-printed titanium implants are anatomically shaped and have precise features to maximize primary stability and promote faster osseointegration. The porous lattice structure on the apical portion is designed so that the bone grows into and onto the lattice structure.
Wedeking says her husband, a clinician placing implants for 20 years, invented the original iDENTICAL implant design based on the advancements he observed in 3D imaging, digital design, and manufacturing technologies. From CBCT imaging, CAD/CAM, 3D printing, and others, he saw an opportunity to create a less invasive procedure with improved patient outcomes by using 3D imaging to design a patient-specific implant.
“Moving toward patient-specific devices is already happening in other body parts. For example, 3D-printed, patient-specific spinal implants have been around for quite some time,” Wedeking says. “Dentistry is finally catching up.”
She thinks it is time for implant dentistry to advance beyond the cylindrical, tapered, screw-threaded design of the past 58 years. “Now is the time to leverage technology to create a new paradigm for implant dentistry: a less invasive, safer, and more personalized process,” Wedeking says. “The core technologies iDENTICAL is leveraging already exist. We are bringing them together with our patented approach to provide the first 3D-printed, titanium, patient-specific implants.”
Many patients have significant fears and anxiety regarding dentistry in general, especially concerning the drilling involved with traditional implant surgery. A drill-free, patient-specific solution can reduce anxiety and barriers to acceptance of treatment plans. Also, Wedeking thinks future clinical studies will show faster osseointegration, which she says will be a huge win for patients. In addition, because the iDENTICAL implant is anatomically shaped and the emergence profile is patient specific, it will improve esthetics.
“The natural gingival contour is fully maintained, which allows the patient to preserve their natural smile,” Wedeking says. “Achieving this outcome with traditional implants in the anterior region can be incredibly challenging.”
Moreover, iDENTICAL reduces the risks associated with implants. “There is virtually no risk of misplacement of the implant or causing nerve damage since there is no drilling required, so it’s a safer process for the patient,” Wedeking explains. “In addition, patients will benefit from the convenience of completing their full implant treatment process in fewer visits, saving time and money.”
Specialists and general practitioners also benefit.
“The cost, time, and effort to invest in these special tools and equipment, learning to use them properly, and properly store, maintain, repair, and replace them can be a significant barrier to placing implants for general dentists. iDENTICAL removes these barriers with its simple system and fully digital workflow,” she says. “Moreover, dentists will benefit from the competitive differentiation gained from showcasing a cutting-edge technology.”
iDENTICAL is in the midst of a clinical trial and is awaiting FDA clearance. However, Wedeking says it is already growing patient awareness and clinical interest in the industry.
“Given the trends of minimally invasive dentistry, digital workflows, advancements in 3D imaging and 3D printing technologies, and the growing aging population, iDENTICAL has major tailwinds in its favor,” Wedeking says. “Now is the prime time to bring iDENTICAL’s technology to the market.”
More Flexibility With Your CAD
Library Means More Design Control
Ruben Arebalo, vice president of Preat, says implant dentistry has pushed toward a digital workflow, which requires digital implant impression-taking. Choosing the correct scan body for the digital impression that works with the abutment the clinician wants for the restoration can be a pain point.
For example, if the clinician uses a scan body that does not work with the chosen abutment, the lab might need a new digital impression. Or, sometimes, the lab recommends a different approach for the restoration that does not match the scan body chosen. Either way, it means getting the patient back for a new impression. Arebalo says Preat’s Choice Library addressed this pain point with scan bodies for any implant by making all abutments in the portfolio available for a digital workflow.
“A lot of times the technician may suggest a different abutment than the doctor selected based off what they see in the CAD software as they’re designing the restoration,” Arebalo says. “Rather than having to rescan, which is a pain, they can just go into their CAD software and select a different abutment. Using the Preat scan body, you have all the abutments in a digital workflow.”
Preat has scan bodies for most implant systems available today. They make a proprietary scan body that is specific to each design. Arebalo says that using one of Preat’s scan bodies, the clinician can scan first and consult with the technician afterward. The restorative team can use a temporary cylinder abutment for a provisional or a titanium base for a screw-retained restoration. The team can also design for a screw-retained restoration with an angled access channel or a custom abutment in their library for a cement-retained restoration if desired. “We open everything up to them from that initial scan,” Arebalo says.
Flexibility also stops implant workflows from little hiccups that cause delays and slow efficiency. Suppose a clinician chooses a screw-retained restoration, and the technician notices the screw access channel in the middle of the facial of the tooth based on the implant placement. In this case, there should be a custom abutment or an angled access channel. However, because of the scan body used in the digital impression, those options were not available for the technician designing the case. Therefore, the process stops until the team determines the next steps. “The scan body dictates everything you could do from a restorative side when using digital impressions technology,” Arebalo says.
The Preat scan bodies’ flexibility reinforces the collaborative concept, which is how Arebalo sees the implant workflow. The clinician and the technician have perspectives that can contribute to the case’s success and improve the patient experience.
“As a prosthetic component manufacturer, we’re just trying to give them all the tools up front to make the best restoration for the patient,” Arebalo says. “Everyone wants to use technology to the patient’s advantage. So, using their digital scanners to speed things up, using the CAD software and milling machines to speed up production on the restorative side. This continues to enable that.”
He anticipates technology further enhancing the workflow. For example, artificial intelligence will undertake preliminary designs for abutments and restorations for humans to review. Also, 3D printing will become part of the implant production process, which is already happening in Europe. Moreover, scanning technology will continue to improve.
“We will continue to see advancements in implant abutments to be even more patient-specific, more driven for that individual tooth site,” he says. “That could be through materials and processes that ask, how do we take something good today and continue to make it better?”
References
1. Thakkar R. Trends in dental implants 2022. American Academy of Implant Dentistry. July 7, 2022. Accessed July 5, 2023. https://connect.aaid-implant.org/blog/trends-in-dental-implants-2022
2. Dental implants market – by product (tapered implants, parallel-walled implants), by material (titanium, zirconium), by end-use (hospitals, dental clinics) & forecast, 2023-2032. Global Market Insights. December 2022. Accessed July 5, 2023. https://www.gminsights.com/industry-analysis/dental-implants-market
3. United States dental implants market report 2023: sector to reach $2.2 billion by 2029 at a CAGR of 6.4%. News release. Research and Markets. March 28, 2023. Accessed July 5, 2023. https://www.globenewswire.com/en/news-release/2023/03/28/2635443/28124/en/United-States-Dental-Implants-Market-Report-2023-Sector-to-Reach-2-2-Billion-by-2029-at-a-CAGR-of-6-4.html
Product Bites – November 10, 2023
November 10th 2023The weekly new products podcast from Dental Products Report is back. With a quick look at all of the newest dental product launches, Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Amann Girrbach, DMG, Pac-Dent, and ASI Dental Specialties. [4 Minutes]
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.
Product Bites – October 27, 2023
October 27th 2023Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Kerr Dental, MGF, PreXion, ZimVie, Amann Girrbach, VOCO, ASI Dental Specialties, DMG, and NovoDynamics. [8 Minutes]