It would be nice if patients took their clinician’s word for it every time regarding diagnosis and treatment planning. Luckily, technology can help you show them while you tell them what’s going on with their oral health, which can help improve patient engagement and adherence.
The Agency for Healthcare Research and Quality says that health care is most effective when patients are knowledgeable about their conditions and what choices are available to them. This understanding makes them actively engaged in their care.1
Plus, they don’t always take the clinician’s word for it. Brandon Thorpe, DMD, a private-practice dentist at Spring Dental of Lumio Dental in Tulsa, Oklahoma, says there’s been a clear shift in patient education preferences.
“Today, patients want to see the problem related to the recommended treatment plan, and they want confirmation and validation from technology,” Dr Thorpe says.
Understanding Your Patient
Managing patient expectations is an essential part of patient education. The Foundation for Oral Rehabilitation (FOR) suggests discussing patients’ oral health goals for a specific treatment. These patient goals should drive the patient education conversation.2
These conversations might also reveal the patient’s overarching goals for oral health. For example, some patients may want to invest only in treatments that alleviate pain, while others may want to maintain or improve esthetics.
FOR offers the following areas to discuss with patients regarding their goals for an upcoming restorative treatment plan and delivery:
Evaluating patient expectations in 4 areas: comfort, esthetics, function, and quality of life. Determine the primary problem, whether they care about what looks best, whether they need to improve their speech or mastication, and whether their self-esteem is affected by the current state of their oral health.
Discovering how far patients want to go with it. For example, do they want full-mouth rehabilitation or wish to concentrate only on the esthetic zone? Is surgery on or off the table?
Determine their professional or personal obligations. These areas might drive their decision-making and affect how they approach the provisional phases of treatment.2
Then, once these factors have been discussed, the clinician should address the following areas in patient education to ensure the best possible outcome with regard to the patient’s expectations:
- What is possible with the proposed treatment and, perhaps more importantly, what isn’t
- The treatment times and timelines, as well as the expected recall appointments
- What it will cost, and what insurance might cover or reimburse
- The patient’s role in long-term success regarding adherence, time, and effort, and, perhaps more importantly, what happens if they do not take that role seriously
- The behavioral adaptations required during and after treatment, including smoking cessation, special diets, and pain management
- The risks to the patient that are associated with the treatment2
Follow Up Expectations Management With Visuals
John Flucke, DDS, chief dental and technology editor for Dental Products Report, says humans are visual creatures. Dr Flucke, who has a bachelor’s degree in psychology, says one of the fascinating things he learned as an undergraduate was that about 87% of what human beings perceive about their environment comes from what they see.
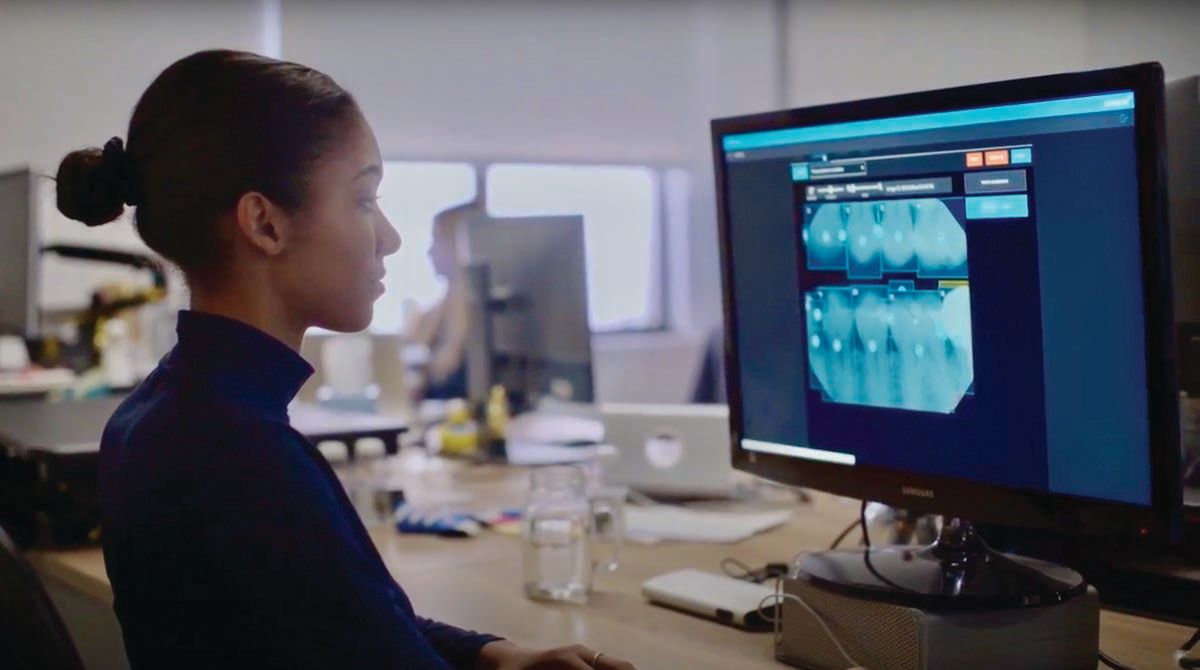
“There’s the adage, ‘I hear, I forget. I see, I remember,’ ” Dr Flucke says. “That comes into play with this. We saw that in dentistry with the advent of digital x-rays.”
He remembers showing patients their dental x-rays through the view box, showing them the decay, and watching them nod in agreement. However, once he showed them digital x-rays of the decay on the monitor, he was astounded by the difference in patient reaction. He jokes that it was obvious that they were lying before when viewing the old x-rays; their new response was so much more engaged with the image of their teeth and gums.
“When you can show it to people on a monitor, it changes things,” Dr Flucke says.
International speaker and mentor Ankur Gupta, DDS, says patients know more about health and dentistry than ever before, which is both a good and bad thing. The problem with being more knowledgeable is that a great degree of skepticism can occur. However, he says clinicians can consistently circumvent suspicion by using high-level photography.
In the past, the problem was that high-level photography came with high costs, both in time and money. Dr Gupta says that when he opened his Ohio practice in 2004, the TV was $2000, the intraoral camera was another $1200, and the SLR cameras were $1000 each. So, high-level photography already cost over $4000.
The higher costs also came in productivity. Since the earlier cameras were not as intuitive as today’s, Dr Gupta was the only one who took the photos, which was inefficient. The actual dollars and the lost productivity due to inefficiency made demonstrating to patients what he saw in their mouths cost prohibitive. Those barriers to entry have gone away, he says.
“Now, you get a TV for $99 on Amazon and mount it in your operatory. Every single operatory can have a TV. You can get an intraoral camera for $300, and an extraoral camera that is so incredibly easy to use and autofocus that anybody, including the least tech-savvy person in your office, can still grab it, point it, and take some nice photos,” Dr Gupta says.
He appreciates how the imagery changes the conversation. Every patient can see what the clinician sees, such as an open or failing margin or teeth that are tipped.
“For me, nothing has ever been as valuable as allowing patients to look at their oral situation closely with a screen in front of them,” he says.
Personalized Recommendations
However, patient education is not just for treatment plans and restorative cases. Patient education is also a critical component of preventive care.
Dental hygiene educator and international speaker Katrina Sanders, RDH, BSDH, M.Ed, RF, says dentistry used to have a one-size-fits-all approach to preventive care back in the 1950s. Everyone used the same toothbrush, paste, and floss.
The many options available today make it harder to choose what’s best. Sanders says hygienists should help patients sort through all the information and products available to create a customized care plan.
For example, patients who have experienced bone loss might have more significant embrasures to clean. Therefore, the hygienist should recommend a specialized tool to address their needs. The same concept applies to patients who lack dexterity or have implants or implant-supported dentures. They need different tools, such as electronic toothbrush heads or water flossers, wooden wedges, or picks, to adapt to the restorations’ surrounding areas.
A Sneak Peek at Where Patient Education May Be Headed
As digital technology continues to evolve, the future of patient education has begun to take shape. Our trio of experts—John Flucke, DDS, Ankur Gupta, DDS, and Katrina Sanders, RDH, BSDH, M.Ed, RF—share more thoughts on how this shift involves digital technology that can help with diagnosis, interpretation, and presentation.
Dr Flucke predicts a future where AI provides treatment planning, but also shows patients just what their smile will look like after the treatment. These applications will also play a role in orthodontic simulations. Not only will this system show patients what they can expect from the treatment, but it can also increase the predictability of the case because the workflow is digital.
“You can print those models that are perfect, and then you can tell the person, ‘This is what we’re going to use to build all of this,’” Dr Flucke says. “So, this isn’t kind of what you’re going to look like; this is exactly what you are going to look like.’”
Looking ahead, Sanders thinks the future of patient education on the preventive side is using salivary diagnostic tests in the dental operatory. Gathering the practical data revealed the test is common practice in medical and even veterinary spaces but not in dentistry. Sanders sees that changing for preventive care, putting salivary diagnostics as a standard part of the dental appointment, alongside x-rays and observations by periodontal probing and the naked eye.
Moreover, having salivary diagnostics alongside the other assessments subject to clinical subjectivity might help clarify the best path forward for the patient’s oral health and identify critical signs of other systemic diseases.
“Salivary diagnostics will start predominating as the assessment tool of choice to get practical, objective data about the concentration of bacteria I see in the patient’s mouth. That gives me a lot of information,” Sanders says, adding that it will also help her choose an oral hygiene modality change that will benefit the patient. “Whatever modalities you prescribe, you can institute the salivary diagnostics on the back end to see if that modality has succeeded. We’re able to evaluate the success of our treatment fully.”
Sanders says the American Academy of Periodontology includes salivary biomarkers and C-reactive protein loads to evaluate patient disease progression on the grading forms. Sanders also acknowledges that some practices already employ salivary diagnostics in their patient care protocols. She thinks these forward-thinking practices are elevating preventive care by screening for diseases and hopes that more dental practices will follow the same protocol sooner rather than later.
Moreover, she says, widespread adoption of salivary diagnostics can help identify bacteria that link to other systemic diseases, which enhances the patient-centric experience customized to individual patient needs.
“Now, we can curate that conversation even more and say, ‘Mr. Jones, you have high levels of Fusobacterium nucleatum, and we now know that this bacterium is implicated in colorectal cancer. Do you have a family history of colorectal cancer? When was the last time that you had a colonoscopy?’ ” Sanders says. “It creates a more personalized conversation that meets not only the patient’s oral health care needs but also their systemic health care needs.”
Dr Gupta, who is a member of the Dental Products Reportâ Editorial Advisory Board, thinks the future of patient education is leveraging social media to showcase one’s practice. Patients will research dental experiences through social media before they call and make an appointment. He says that dentists who will be well positioned are already embracing it and have a social media presence.
The content doesn’t have to be elaborate, he says. Explaining what a crown or cavity looks like when drilling on it are examples of what a clinician could include. Right or wrong, Dr Gupta, says these presentations could be how patients differentiate a dentist who knows what they are doing from a dentist who doesn’t.
“That’s not fair, and it’s not accurate, but that type of perception will be more rampant,” Dr Gupta. “If you’re going to explain what a cavity is to your patient in the chair, you might as well explain it to your phone so you can post it on your social media.”
- by Terri Lively
She thinks these changes are great for patient care. However, it can also be a lot for patients and oral health care providers.
“The range of what oral hygiene care products looked like in the 1950s to what we would consider to be an oral hygiene care product today has very much expanded in an exciting way,” Sanders says. “But it can also be overwhelming.”
What Technology Is Changing
Dr Flucke thinks that the next big moment in patient education will happen via artificial intelligence (AI). In his office he uses Pearl’s Second Opinion, an AI tool that analyzes x-rays. The color-coded areas of the x-ray are where the AI has identified various oral health conditions.
“When you can show somebody an x-ray, that’s one thing,” Dr Flucke says. “But then, when you can show them an x-ray and say, ‘this is the x-ray, and here’s what Second Opinion thinks, and these pink areas show up,’ or whatever color for the type of problem you are wanting to educate on, people can readily see that.”
AI provides 2 things in this scenario, he says. First, it makes it easier for the patient to see. Second, it gives more information, so patients understand there is a problem. Too often, patients equate no pain to no problem in their oral health; however, that isn’t always the case.
“As I’ve said for a couple of decades now, better-informed patients make better decisions,” Dr Flucke says.
“Simplicity is critical in this process,” Dr Thorpe agrees. “Technology like VideaHealth’s dental AI software, digital photography, and intraoral scanning is helping our team provide greater transparency for patients and uncomplicated visualizations of areas of concern. With dental AI, it is like having a secondary expert opinion alongside you during patient interactions, which helps boost patient trust.”
Assessments involving intraoral scanning and case presentation with VideaAI are concise and easy ways to help patients understand what is happening inside their mouths, Dr Thorpe says. All of this adds up to an improved patient experience that brings more trust to the relationship because clinicians are helping patients better understand the “why” behind their treatment recommendations.
“Dental AI allows patients to co-diagnose in a way, as they are more engaged in the process, asking, ‘What is the red box/yellow circle?’” he explains. “All of this leads to increased treatment acceptance and, ultimately, better patient outcomes.”
Also, 3D imaging makes a significant impact on patient education. Dr Flucke thinks that the ability to show patients on a screen the oral condition from every angle adds to their information. Also, using a time-lapse feature for a series of scans over a period can demonstrate to patients what’s happening in their mouths. This feature is excellent for educating the skeptics, Dr Flucke says. It shows patients in an objective way the wear and tear that occurs in the oral cavity over time.
“I love the expression, ‘I don’t fix the blame; I fix the problem,’” Dr Flucke says. “Sometimes people feel judged. But I tell them that ‘This is a judgment-free zone. I’m going to tell you what I see, what I think you need, and we’ll go from there.’”
Technology Helps Change the Conversation, Too
Regarding preventive care, Sanders thinks smart toothbrushes from the manufacturers help the clinician get more involved in the patient’s success with their home care. The data collected from patient brushing reside in the app, allowing hygienists to observe some details. For example, the data include how long and how often patients are brushing, how efficient and effective they are, and how much pressure they use with the brush.
“It has been terrific,” Sanders says. “The technologies that help educate the patient on how they are delivering self-care as a way of helping to maintain the level of work that we do in the operatory also really gives us a leg up in understanding how to support the unique challenges each patient may have in their home care.”
For example, when discussing self-care, the data in the app open up the dialog between clinician and patient and put the conversation back in the patient’s hands. The data also empower patients to take control of their oral health and help clinicians educate them on how their actions affect their oral health.
“Most patients know you should be brushing and flossing your teeth and gums, and yet data points remind us that that is not enough to move most patients to deliver the self-care they need,” Sanders says. “So now these technologies help the patient understand. If they come in for that 6-month hygiene visit and things don’t look good, we can look back at the things that they’ve been doing over the past 6 months and ask them, ‘Has that been serving your oral health, or has that been influencing the level of disease that I see today?’ ”
Patient education happens outside the dental chair, too. Dr Gupta employs the help of a subscription platform called Channel D. Through an app, Channel D produces funny and entertaining videos about dental issues and oral health that play in the waiting room. The content covers topics like explaining implants, what a cavity is, and why patients grind their teeth at night. In addition, the Channel D team can add Dr Gupta’s social media videos and incorporate photos of him and the team into the graphics.
“They superimpose my picture on the animated doctor. It looks like I produced them, but I didn’t,” he explains. “These videos are done in a way that they’re very highly entertaining and they prompt a lot of patient engagement.”
Where Patient Education Is Heading
Dr Thorpe sees the future of patient education taking shape now and says it involves digital technology that can help with diagnosis, interpretation, and presentation.
“It will be a system that uses a mix of intraoral photographs/full arch scanning/x-rays plus AI to efficiently interpret and consolidate findings into a concise and easy-to-read visual representation for the patient,” Dr Thorpe says.
Dr Flucke also sees a future where AI provides treatment planning. Moreover, it can show people what their smile will look like after the treatment.
He also sees similar applications for orthodontic simulations. Not only will this show patients what they can expect from the treatment, but it can also increase the predictability of the case because the workflow is digital. The same data for the simulation will be what the dentist uses to build the case. As dentistry moves forward, treatment planning can demonstrate exact results instead of the clinician’s best guess.
References