How to ensure radiation exposure is limited for pediatric patients
Strategies and approaches to protect your youngest patients who are the most vulnerable to radiation exposure.

Recently, there is an increase concern in the public and health professionals about exposure to radiation (medical and dental) in children. In 2007, the International Commission on Radiation Protection changed the calculation of the effective dose from ionizing radiation, and this change revived interest in the concept of As Low As Reasonably Achievable (ALARA).
The individual risk from dental imaging is small when compared to the benefits it can provide through helping with accurate diagnosis. Still, unnecessary radiation exposure during dental procedures should be avoided. This is critical in children. Children are more sensitive to radiation. They have more rapidly dividing cells that can be exposed to low-level of radiation. The main goal of this article is to understand the importance of radiation safety in the practice of dentistry with children and important measures to attain this goal.
Children are more sensitive to radiation
In comparison with adults, children are inherently at greater risk of cancer induction from radiation exposure. Sensitivity to radiation is higher early in life. The greater sensitivity in children is probably related with a rapid cell division in developing tissues.
The radiation exposure from a single dental diagnostic procedure is usually small. Because of the increased
lifetime risk per unit dose for children, the potentially higher doses, and the increasing frequency of pediatric radiology procedures-including dental procedures-can lead to a small, but non-negligible, increase in risk of cancer. While these procedures are clearly beneficial, the magnitude of exposure of children can often be reduced with- out significant loss of information.
The Alliance of Radiation Safety in Pediatric Imaging is a coalition of different and numerous health care organizations dedicated to providing safe, high-quality pediatric imaging.1 The main mission of the Alliance is to create and increase awareness in the imaging community of the need to adjust radiation dose when imaging children.
Trending article: How to get the perfect X-ray for you
The Image Gently Campaign®
The American Academy of Oral and Maxillofacial Radiology, the American Academy of Oral and Maxillofacial Pathology, The American Academy of Pediatric Dentistry, The American Dental Association, the American Association of Oral and Maxillofacial Surgeons, The American Association of Endodontists and The American Association of Orthodontists are part of the alliance. The Image Gently Campaign in dentistry focuses on improving safety and effectiveness in pediatric imaging of the maxillofacial complex by informing dental professionals and parents about radiation safety best practices. The campaign outlines seven steps during pediatric dental procedures:
- Select x-rays for individual needs, not merely as a routine
- Use the fastest image receptor possible
- Collimate the beam to areas of interest
- Minimize retakes
- Always use thyroid collars
- Child-size exposure time
- Use cone-beam CT only when necessary
Trending article: How to improve diagnostic accuracy while lowering radiation dose
Justification for radiation exposure
Justification refers to the pertinence of each radiograph performed. There are no limits in the exposure when there is a clear justification. The clinician has the responsibility to assure each exposure is justified. If the image is indicated, there are no limits or restrictions on patient exposure.2
In the pediatric patient, as well as with adults, radiology is part of the diagnostic process, but it is not the only piece of the diagnostic diagram. The decision is made on the findings from the patient history, clinical examination, and review of any previous radiograph. Critical is also the particular circumstances of each patient. For example, a bitewing radiograph is probably not justified in a child with posterior open contacts. The critical point is the dentist must take the individual characteristics of the patient into account when making radiography decisions.
The anticipated individual benefits must be that the radiographic examination is likely to add new information to the patient’s treatment. The American Academy of Pediatric Dentistry endorsed the selection criteria guidelines published by the American Dental Association.3
Continue reading on page two...
Using the optimal X-ray receptors
The adoption of digital intraoral imaging receptors-solid-state sensors and reusable phosphor plates-has been slow but steady in the United States. These faster receptors have been adopted primarily to reduce patient dose, improve overall image quality by eliminating chemical processing and to increase office productivity, which are all positive goals. It is recommended that all dental practices should adopt digital intraoral X-ray imaging.
Solid-state sensors and reusable phosphorous plates will reduce patient X-ray dose the most, compared with conventional films.3 Reusable phosphor plates (PSP) are similar in size to the conventional films. In young patients, PSPs can be easier to position in the oral cavity and more comfort- able for the patient. Furthermore, PSPs are associated with fewer retakes in the young patient, which translates to less radiation exposure.
Unfortunately, because the images from solid-state detectors can be seen immediately, it is recognized that many operators often take multiple images in order to select “the best” when working with solid state sensors. This practice defeats the intent of reducing dose to the patient.
All dentists in all dental practices must re-educate and instruct their dental assistants in proper positioning techniques and safe radiographic imag- ing practices to eliminate retakes and reduce patient X-ray dose. In 2006, it was estimated by an NIDCR committee looking for large data sets for research in osteoporosis, there were approximately 750,000,000 dental X-rays performed annually. It is estimated the number would be well over 1 billion dental X-rays annually now. It has also been reported that 7 to 13 percent of all dental X-rays are retakes. That means that there are more than 100 million unnecessary dental X-rays taken every year in the US. This is a conservative estimate that only documents the known retakes.
Trending article: Making the switch to digital radiography
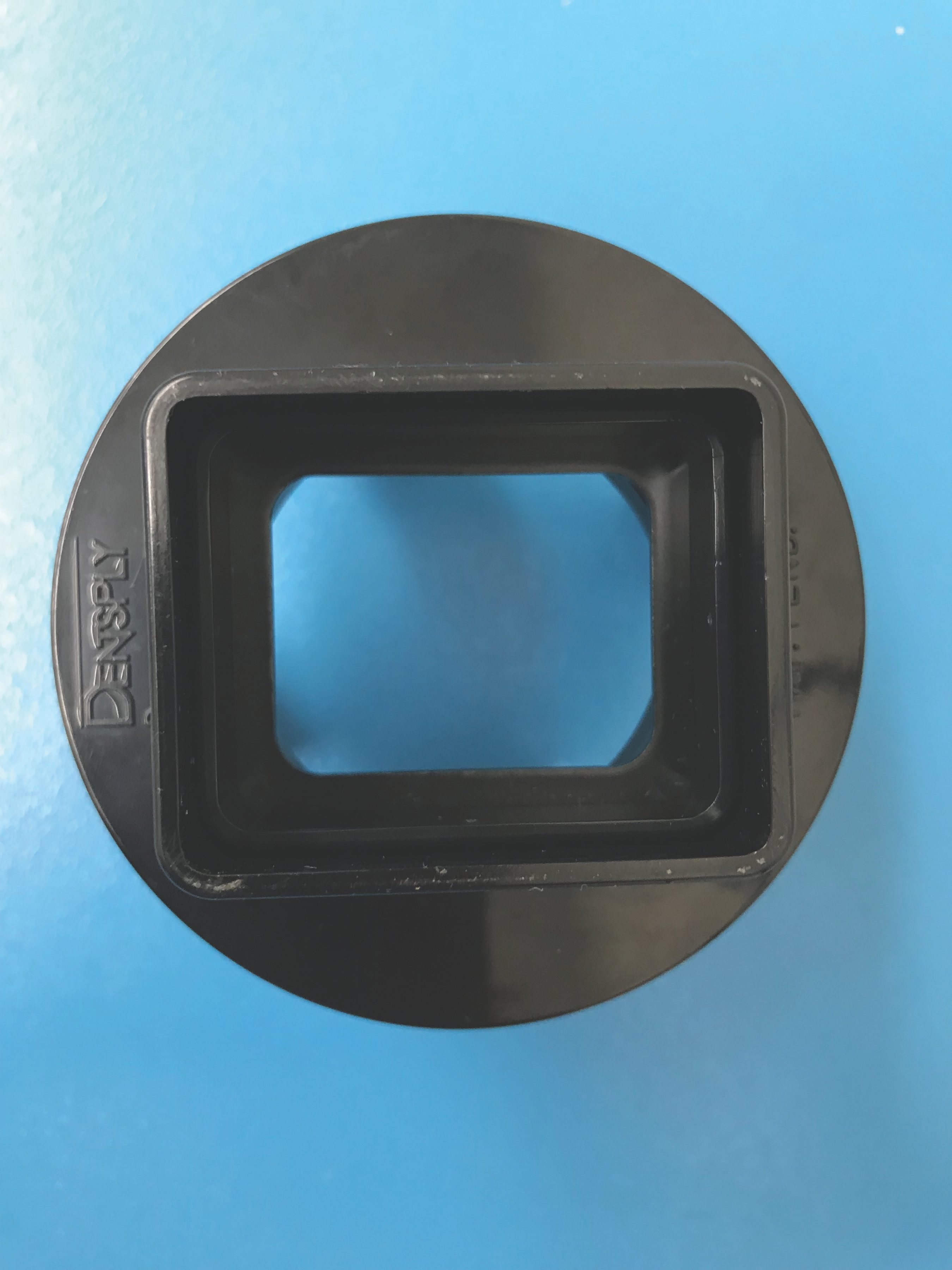
Fig. 1: Rectangular collimator side view
The benefits of rectangular collimation
Several ways to limit the size of the X-ray beam are available. The National Council on Radiation Pro- tection and Measurements (NCRP) Report 145 (2003) provides radiation protection guidance for the use of X-rays in dental practice.4 The NCRP was chartered by the U.S. Congress in 1964 to perform several tasks related with the use of radiation, including to periodically assess new technologies and radiation safety practices in order to make recommendations.
By following the report, dentists and patients can obtain maximum benefit and minimum radiation exposure. Rectangular collimation has been widely available for several decades. Several U.S. dental schools recommend the use of rectangular collimation. However, there is not a significant acceptance in the dental office.
Using the appropriate collimation to the precise size of the image receptor eliminates scatter radiation. When scatter radiation hits the receptor, the result will be a reduction in image quality. Most companies produce large, round cones with large X-ray beam patterns so the operator will be sure to expose the film or receptor.
Round collimation adds scattered radiation, decreases the image quality, and increases the patient radiation dose. The NCRP Report 145 suggests rectangular collimation of the beam be used routinely for periapical radiography.5 Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimen- sion of the image receptor by more than 2 percent of the source-to-image receptor distance.
Fig. 2 Rectangular collimator bottom view

There are several advantages of rectangular collimation over round collimation in terms of reduction of the radiation dose to the patient and increased contrast and clarity of the image. The general reduction of the effective dose using rectangular col- limation is close to 35 percent.
Hot read: 5 surprising ways digital tools can boost your abilities
The other advantage of rectangular collimation is the reduction of scatter radiation and the increase of the image contrast. Scattered radiation adds unwanted and non-diagnostic photons to the image and that decreases the contrast. Peterson and collaborators compared the image quality between bitewings taken with rectangular collimation and round collimation in terms of caries detection. Results showed the films taken with rectangular collimation ranked higher for film resolution, overall appearance and accuracy of caries diagnosis.6
There are reports that suggest the use of rectangular collimation may result in more retakes. Thornley et al looked at the retake level using rectan- gular collimation in a group of general practitioners. They found the use of rectangular collimation increased the number of retakes by 7 percent with a significant reduction in the radiation dose to patients.7
Parrott and Ng studied if the use of rectangular collimation was associ- ated with cone cut errors that could adversely affect the diagnostic capabil- ity of the film. They found that the use of rectangular collimation increased the incidence of cone cuts.8 However, the errors considered “rejects” was very small. They also concluded that use of film holders helps in reducing the incidence of errors. Parks also looked at the errors produced by the use of rectangular collimation and found more errors are associated with the use of rectangular collimation. However, the majority of errors were not signifi- cant enough to generate a retake.9
Continue to page three for more...
Converting to rectangular collimation
Several methods are available to con- vert an existing round collimation into rectangular collimation. Probably the easiest is by inserting a rectangular collimator at the end of the round cone (Figs. 1-4). The other two methods include the use of rectangular cone or the use of a position-indicating device with the round cone and which collimates the beam at the skin surface.
Collimating the X-ray beam does not affect the settings for conventional or digital films. It is important to reaf- firm the critical role of film-holding and beam-alignment device to decrease the frequency of errors including cone-cuts and retakes. Several dental companies offer different options to convert existing round collimation into rectangular collimation.
Related reading: Why responsible pediatric dental radiology is a must

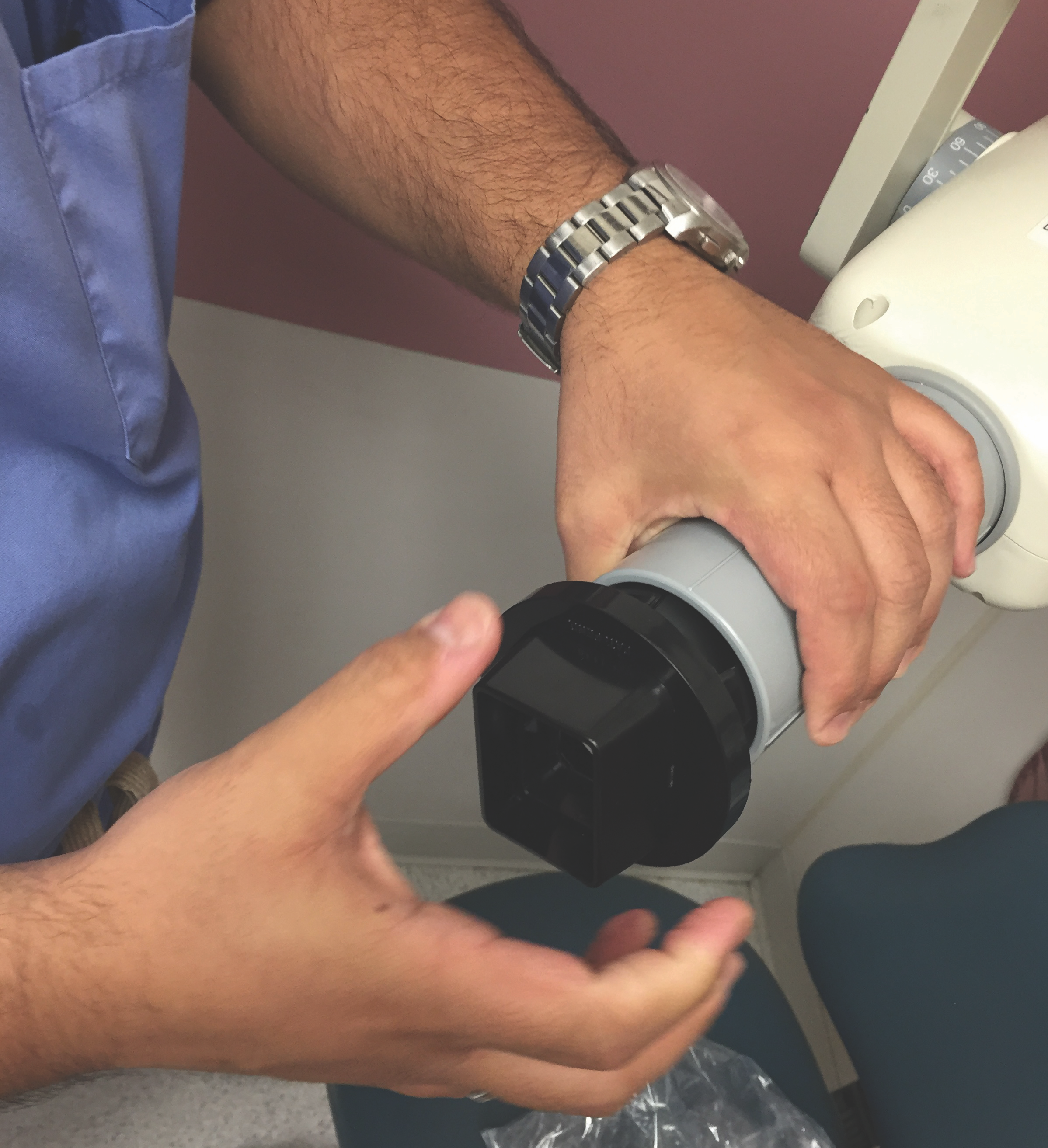
Figs. 3 & 4: Insertion of the rectangular collimator at the end of the round tube
Conclusion
Radiographs are critical components of the diagnostic process. However, the use of X-rays carries a small risk of radiation exposure. Children are more radiosensitive than adults. Decreasing radiation exposure to children and producing consistently high-quality radiographic images are critical goals of any dental office.
Several organizations, including the American Dental Association and the American Academy of Oral and Maxillofacial Radiology, recommend the use of rectangular collimation for periapical and bitewing radiographs in order to reduce further radiation exposure and dose to children. The use of PSP in children is advised, similar size to conventional films and easy positioning in the mouth are factors that decrease the number of retakes.
Even with clear advantages in terms of dose reduction and better image quality, rectangular collimation has not been widely used in practice. Critical issues related with an easy transition to rectangular collimation include the use of positioning devices, use of rectangular collimators that can be inserted at the end of round tubes and the review of the paralleling technique.
Dentists are responsible for protecting children from excessive radiation by regularly updating the equipment, reexamining practices and techniques, and following recommendations for standards of care. Further studies must look at the specific reasons of the underutilization of rectangular collimation and creating strategies to increase use.
References
1. Don, S., et al., Image gently campaign back to basics initiative: ten steps to help manage radiation dose in pediatric digital radiography. AJR Am J Roentgenol, 2013. 200(5): p. W431-6.
2. White, S.C. and S.M. Mallya, Update on the biological effects of ionizing radiation, relative dose factors and radiation hygiene. Aust Dent J, 2012. 57 Suppl 1: p. 2-8.
3. Seale, N.S., AAPD Clinical Practice Guidelines- -why they are more important than ever. Pediatr Dent, 2013. 35(5): p. 404-5.
4. Miles, D.A., et al., NCRP report No. 145: New dental X-ray guidelines: their potential impact on your dental practice. Dent Today, 2004. 23(9): p. 128, 130, 132 passim; quiz 134.
5. Basic anatomical and physiological data for use in radiological protection: reference values. A report of age- and gender-related differences in the anatomical and physiological characteristics of reference individuals. ICRP Publication 89. Ann ICRP, 2002. 32(3-4): p. 5-265.
6. Peterson, C.A., et al., Effects of beam collima- tion on image quality. J Dent Hyg, 1997. 71(2): p. 61-70.
7. Thornley, P.H., et al., Rectangular collimation and radiographic efficacy in eight general dental practices in the West Midlands. Prim Dent Care, 2004. 11(3): p. 81-6.
8. Parrott, L.A. and S.Y. Ng, A comparison between bitewing radiographs taken with rectan- gular and circular collimators in UK military dental practices: a retrospective study. Dentomaxillofac Radiol, 2011. 40(2): p. 102-9.
9. Parks, E.T., Errors generated with the use of rectangular collimation. Oral Surg Oral Med Oral Pathol, 1991. 71(4): p. 509-13.

Product Bites – November 10, 2023
November 10th 2023The weekly new products podcast from Dental Products Report is back. With a quick look at all of the newest dental product launches, Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Amann Girrbach, DMG, Pac-Dent, and ASI Dental Specialties. [4 Minutes]