Hype vs. Reality: Is New Dental Technology Changing the Game
"Game changer" gets thrown around a lot regarding new dental technology. We look at the reality of dental technology.
Hype vs. Reality: Is New Dental Technology Changing the Game. Image courtesy of Who is Danny/stock.adobe.com.
Marketers like to throw around the phrase "game changer" in conversations about new dental technology. They need your attention, so they do their best to get it by creating attention-grabbing content and splashy advertising campaigns.
But does the reality of dental technology live up to the hype? We look at dental technology today, including materials science, laser dentistry, 3D printing, artificial intelligence (AI), and robotics.
Hype vs Reality
John Flucke, DDS, technology editor for Dental Products Report®, thinks that the individuals selling dental technology always claim they have something that is going to change the world. It’s the dentist’s responsibility to maintain a stance of healthy skepticism and do the research.
That said, Dr Flucke says technology has been great for dentistry. It allows clinicians to streamline and do things more efficiently. “It has changed society’s view of dentistry,” he says.
Marty Jablow, DMD, chief development officer for Cellerant Consulting Group, agrees that adding technology changes the way clinicians practice. Dental technology today facilitates complicated treatments and procedures, from guided surgery and 3D printing of restorations in the office to making a crown and sliding it under a partial denture. “Things that I thought were impossible 10 or 15 years ago are now routine,” Dr Jablow says.
Dr Flucke also appreciates how things change constantly, even the little things, to make dentistry better. Plus, he loves what he does. “The neat thing about being a clinician is you don’t end up doing the same thing over and over again. You get to learn and evolve, and the patients get the benefit of that in the end,” Dr Flucke says. “As things change, we don’t go backward. We go forward and make progress, and progress is always good for health care.”
Understanding the Reality of Dental Technology Today
Dental technology is only as good as the individuals using it, Dr Jablow says. Training is a must. Clinicians can’t complain about equipment not living up to the hype if they haven’t learned how to take full advantage of it. For example, scanning an arch with an intraoral scanner requires technique. Otherwise, a clinician will introduce errors into the scan. “It’s not the machine that’s causing the problem,” Dr Jablow says. “It’s the inadequate training to do it properly.”
To uncover the reality of dental technology, Dr Jablow says clinicians should lean on the manufacturers. No one knows the product like they do. Also, third parties can direct you to better types of equipment and work with the manufacturer to expand the training that comes with them.
Clinicians should know the realities of adopting new technological workflows. For example, technology can handle digital treatment planning and print a mock-up in the office quickly. However, this workflow requires trained staff and a place to do it. Little things are different, too. For example, postprocess resins introduce new smells in the office.
Part of the problem with too much hype is the language used to describe dental technology functionality. For example, common phrases such as “handles the dental process for you” or “with the push of a button” create unrealistic expectations. “The only ‘push of a button’ is to turn the thing on. After that, technology requires interaction [with] the dentist, staff, and software and the ability to pull it all together. You can’t just push the button,” Dr Jablow says. “It’s not the elevator.”
Dr Jablow encourages clinicians to hear feedback about dental technology from end users and key opinion leaders (KOLs). Additionally, online forums for individuals who use dental technology are valuable to see who is having problems and who is doing well. Most importantly, Dr Jablow says it is critical to know what you want the technology to do. “Without the foresight as to what it’s going to do for you, a practice usually ends up with a piece of equipment in the corner of the room,” Dr Jablow says.
Dr Flucke encourages research as part of the healthy skepticism stance. He uses 3 criteria to guide his research:
- Does it give me an equivalent or better result than what I use now?
- Can I spend less time doing something, optimizing my appointments and ergonomics?
- Is it affordable?
The last criterion bothers Dr Flucke a little. He hates to talk about money when it comes to health care. However, affordability is an essential consideration, especially when a dentist is wearing their small-business owner hat. “You can be the best dentist in the world, but if you can’t stay in business, you won’t help anybody,” Dr Flucke says.
What’s Real About Materials Science?
Michael A. Miyasaki, DDS, a dentist in private practice in Sacramento, California, agrees with Dr Flucke that healthy skepticism is essential, especially in materials science. However, Dr Miyasaki thinks clinicians should have enough bravado to leave their comfort zone and try new products.
Dr Miyasaki also agrees that feedback from peers or from respected KOLs can help. Dr Miyasaki says the RE-GEN™ bioactive composites from Vista Apex that were developed with John Kanca III, DMD, got his attention because he respects Dr Kanca’s expertise. Dr Kanca’s involvement and an understanding of the science behind the product helped Dr Miyasaki become comfortable using this material in his practice and recommending it to other clinicians.
Regarding bioactive materials, Dr Miyasaki doesn’t think the excitement surrounding them is hype. He thinks bioactive adhesives and liners will enhance the longevity of restorations and could prevent invasive restorative work such as crowns and implants later in the patient’s life.
Rolando Nunez, DDS, MSc, manager of clinical research at BISCO, Inc, says the hype surrounding CAD/CAM materials is widespread. Marketers often describe materials as the next best thing without enough substantiation to make that claim. His response is to test the materials by bonding to them, seeing how they react to different conditions, and comparing these data with the claims the companies make.
Materials manufacturers are following a trend to have as many indications for their product as possible, Dr Nunez says. They market this versatility to clinicians who buy the product in hopes of reducing the practice’s armamentarium. However, Dr Nunez says there isn’t 1 product that can do it all. When materials don’t work for all indications, the restorative outcome has poor consequences for the patient experience and the manufacturer’s reputation.
To avoid this outcome, Dr Nunez say it isn’t wise to purchase materials from unknown companies. This could mean buying a suboptimal product from a company that doesn’t specialize in that area of dentistry. “Use a product from a reputable company that has a history of developing restorative materials and bonding agents,” Dr Nunez says.
Lisa Jeong, director of marketing at Tokuyama Dental America, Inc, says perfectionism is part of the problem, especially regarding matching shades. No composite is a perfect match, and shade-matching technology is always a little different from the natural tooth, she says. “They expect it to be 100% perfect and [that] the composite should match the dentin, enamel, and different gradations of teeth,” Jeong says. “And 90% of the time, it can. But it’s tough for it to be 100%.”
Jeong says the same challenge exists for the universal application of composites. For example, in the posterior teeth, clinicians need strength, but in the anterior teeth, they need esthetics. Universal composites will be very good in both categories but not perfect. Additionally, the definition of perfect has some variation. What is perfect to one clinician isn’t perfect to another.
To prevent disappointment, Jeong encourages clinicians to try products before they buy them to see how they work in their hands and determine whether they have a place in their inventory. Each time a manufacturer comes out with a product, Jeong says, it improves over the one before. Testing new products is essential so clinicians can see for themselves whether the improvements will benefit their practice. “Practitioners should realize a universal or unishade will help them and make their lives easier,” Jeong says. “But at the same time, it’s not going to be perfect.”
Ron Nolan, vice president of marketing for Solmetex™, says advances in the dental materials area have come very quickly. Although the fundamental practice of dentistry hasn’t changed a lot, applying the material has. Nolan is a huge fan of a dental professional’s self-study to invest in their knowledge of improvements in materials and techniques.
That same strategy should apply to infection control best practices, Nolan says. By leveraging the guidance and regulations from governing bodies such as the Organization for Safety, Asepsis and Prevention (OSAP), the US Environmental Protection Agency (EPA), and the US Food and Drug Administration (FDA), dentists can establish their protocols. “Dentists take their practice and its responsibilities very seriously,” Nolan says. “Because they see so many patients every single day, things like infection control are very high on their list to provide proper point of care.”
Although infection control is a high priority, Nolan recognizes that it is also a burden to dental practices. Staying within the protocols has a technology component to it, which dental practices can leverage to their benefit. For example, Solmetex designed the NXT Hg5 Amalgam Separator to meet or exceed all state and federal requirements for mercury removal and recycling. Additionally, they host the Solmetex Compliance Program so dentists can access their documentation and autoship containers depending on the practice’s needs for replacement. “We like to make sure that we keep [clients] up-to-date,” Nolan says. “We have over 100,000 [clients whom] we support.”
In addition, Sterisil® and Solmetex are the only companies that provide an end-to-end continuum of care for dental unit waterlines that comply with the EPA and OSAP recommendations. They reduce bacteria levels below EPA regulations (500 ppm) to almost 10 ppm. Additionally, the company provides in-office and mail-in tests and the required documentation to verify the practice’s protocols. “We’re the only company that adheres to OSAP and ADA (American Dental Association) recommendations,” Nolan says. “Most doctors are stewards of the safe patient environment in their practices and will test for their own purposes to verify that their protocol is working. You have to admire them for that.”
The Reality of Laser Dentistry
Samuel B. Low, DDS, MS, MEd, vice president of dental and clinical affairs and chief dental officer of BIOLASE, Inc, says there is a lot of hype around the bridge between technology and health care, especially oral health care, as new devices and systems continue to evolve. At the forefront is laser dentistry technology, which has revolutionized both patient care and outcomes, he says.
From restoring and repairing dental hard and soft tissue anatomy to alleviating pain and reducing fears and anxiety, Dr Low says laser dentistry improves patient quality of life and elevates the practice of dentistry. When you combine dental laser technology with provider expertise, the standard of care is enhanced for quality patient care, he explains. “As the world’s top innovator in dental lasers, BIOLASE is leading the industry by making procedures user friendly, safe, efficient, and time-effective with a line of award-winning all-tissue and soft-tissue lasers used for minimally invasive procedures and treatments including endodontics, periodontics, dental implants, restorative dentistry, soft tissue, and more,” Dr Low says.
Caitlin D’Entremont, director of product marketing for Convergent Dental, the maker of Solea, says the vastly improved patient experience and clinical outcomes with Solea back up the hype surrounding laser dentistry. The Solea All-Tissue Dental Laser delivers anesthesia-free, blood-free, and suture-free procedures, offering a completely different experience for both dentists and patients compared with traditional instruments and even other lasers.
When it comes to cutting teeth, the more efficiently the laser’s wavelength is absorbed, the faster and more precisely the laser cuts. Solea has a 9.3-μm wavelength that is highly absorbed in tooth structure, specifically in hydroxyapatite and water.
“Solea vaporizes enamel, unlike other lasers that slowly chip it away. This gives dentists a much faster and smoother cutting experience,” D’Entremont says. She adds that Solea is the only CO2 laser cleared by the FDA for all tissue indications.
Consulting with company representatives and speaking to and learning from successful laser dentists help uncover the reality about laser dentistry. D’Entremont says manufacturer representatives know their products inside and out, so they often understand the benefits of their laser and how it can fit into specific practice needs. Successful laser dentists have the clinical experience and practice implementation understanding that can be beneficial to those looking into laser dentistry.
Moreover, experienced laser dentists can describe firsthand how laser dentistry has benefited their patients and practice. Joshua P. Weintraub, DDS, PA, a dentist in private practice at Stevenson Smiles in Stevenson, Maryland, has been a Solea laser dentist for 8 years and an erbium laser dentist for 6 years before that.
“After integrating Solea, it did not take long before I was performing more than 90% of cavity [preparations] without anesthesia vs around 30% with erbium. I am routinely doing soft tissue work without anesthesia, bleeding, sutures, or postoperative discomfort. Flapless osseous crown lengthening surgery is a breeze, as Solea cuts with unparalleled precision and efficiency,” Dr Weintraub says.
Same-day dentistry is also now possible thanks to the laser. The minimally invasive procedure and clean surgical site allows for the completion of a crown in a single visit. Dr Weintraub says his patients and staff are blown away by what Solea can do.
“You can perform soft and osseous tissue surgeries, from gingival contouring to implant uncovery, you may have previously referred out,” Dr Weintraub says. “Patients are happier with [fewer] appointments, and you [can do] an extra procedure you weren’t necessarily planning on that day.”
Dr Low also encourages dental professionals to remain committed to learning and refining their abilities to enhance patient care, elevate their practice, and remain competitive. “Take dental education and training courses, read articles and testimonials, talk to colleagues, inquire about [things], and utilize new technology such as the Waterlase iPlus, Waterlase Express, Epic X, or the Epic Hygiene to be aware of new, innovative ways to approach treatments and procedures. Hands-on events and opportunities are key, as professionals can experience for themselves and see the reality and multitude of benefits [from using] dental lasers,” Dr Low says.
“Education and learning from peers [are] such important aspect[s] of practicing medicine in general,” Dr Weintraub agrees. “I have had the good fortune of learning from some outstanding laser dentists over the years and now have the privilege of educating those who adopt this remarkable technology.”
The dental industry is moving from strict reliance on invasive procedures with manual instrumentation, according to Dr Low. Although traditional methodologies have been successful in the past, they were more invasive and not time-effective. Dental anxiety and fear are real, Dr Low explains, but thanks to advancements in technology, the industry has embraced more patient- and provider-friendly alternatives. “With current appreciation of the expanded innovation of dental laser technology, enhanced capabilities result in reduced time in the chair, less dependence on local anesthesia, and better patient outcomes overall,” Dr Low says.
“Having had experience with multiple different lasers over the years, I can tell you the hype [about] laser dentistry is finally real, when it wasn’t 10 years ago,” confirms Dr Weintraub. “I cannot imagine practicing without my Solea, and my patients will never accept traditional dentistry again.”
3D Printing Has a Multidimensional Reality and Fantastic Future
Lisa Aguirre, dental marketing manager for Roland DGA, says the reality of 3D printing is that the technology is low-cost and generates a quick return on investment (ROI), especially on items such as splints, night guards, and models. However, the hype around 3D-printed materials falls short of reality as a permanent restorative solution. The materials today, even those cleared by the FDA as permanent 3D-printed materials, do not perform as well as analog and milled materials the industry has come to trust over the years. “The hype is in the cost, as these materials can 3D-print permanent restorations for pennies on the dollar. But clinical findings show those materials are not standing up like traditional analog and milled materials,” Aguirre says.
3D printing systems bolster digital workflows, creating a more efficient dental practice or lab. As part of this, it’s important to understand 3D printing’s current capabilities and the difference in digital materials and analog materials. This understanding will allow clinicians to make the best decisions for their patients and practice.

For example, some patients with a traditional denture made from conventional acrylic materials have had it for 20 years. Aguirre says you will not see a 20-year-old printed denture. The remedy for this short life span is to print another one, but Aguirre thinks patients will still feel less confident in their appliance when they know it won’t last as long as a traditional denture. “Any time you have to redo something, even if it doesn’t cost them anything, there’s a patient confidence factor lost there,” Aguirre says.
Therefore, Aguirre encourages clinicians to have realistic expectations about what they can do with a 3D printer and what they can’t. Identify realistic applications in the short and long term. For example, clinicians who want to have an optimal ROI with 3D printing should consider printing splints, night guards, and models in house in the short term. “That’s going to be part of their everyday bread and butter and make for an easy ROI,” Aguirre says.
Guillaume Bailliard, president of health care at Formlabs, says that chairside 3D printing is in a phase of early adoption. Currently, the adoption rate is approximately 5% to 10%. “The reality is we’re still [in] an early phase. There are a number of applications now, and they’re growing. You can do restorations, surgical guides, mouth guards, indirect bonding trays, a lot of different potential applications. So 3D printing is here to stay,” Bailliard says.
The excitement around the potential for 3D printing has created a noisy environment for clinicians, with many 3D printer manufacturers jumping into the market, Bailliard says. However, he recommends that clinicians do their homework about what is purchased and used in clinical practice. Also, he would urge clinicians to look at clinical evidence that validates their utility in a dental practice. “You have to look at the company and peel the onion back to see what resources are behind the company,” Bailliard says about 3D printer manufacturers.
For example, Bailliard recommends asking some questions during your research. Is the company going to be around and have the resources to further develop applications on your existing printer? Does the printer you are buying have a long-term ROI but also meet basic biocompatibility requirements that are needed in any medical field, including dentistry?
“Unfortunately, you have to go beyond the marketing and look behind closed doors, listen to your peers, look at the clinical evidence and the company. You have to do your homework,” Bailliard says. “That’s why we invest in a lot of clinical studies at Formlabs.”
Formlabs recognizes that medical and dental health care have unique needs. They recently created a health care unit that focuses on solutions for dentists and medical providers as part of a broader company approach that serves other vertical markets. The idea is to create seamless workflows that make it possible for dental practices to have a mass adoption of 3D printing.
“We know we have to be able to deliver industry-leading print quality,” Bailliard says of his division. “If you print a temporary crown super fast but it doesn’t fit, that doesn’t do you any good. You have to be able to provide accuracy in your prints.”
Replacing AI Science Fiction With AI Reality
We hear a lot about AI these days and not only in the movies. In dentistry, AI is living up to the hype in many ways.
Although Ophir Tanz, founder and CEO of Pearl, thinks the core detection technology has arrived for 2D imagery and that AI has potential to be a real game changer, the reality of AI in dentistry is that covering all potential use cases will be a moving target. Like author William Gibson’s commentary about the future, Tanz says the future of dentistry AI is here—it’s just not evenly distributed yet.
Nevertheless, Tanz thinks AI could elevate the level of patient care to a point higher than it has even been before. “In our case, the Pearl technology surfaces 37% more disease per radiograph encountered that was not diagnosed by practitioners,” Tanz says. “It’s clear that dentists could benefit from significant assistance in this area, and there’s been no real way to provide that assistance ahead of this technology.”
To get to this point in AI dental technology development, Tanz says 3 things had to happen:
- Capabilities needed development to be useful.
- Requisite regulatory clearances needed to occur.
- Adoption needed to yield satisfied customers.
After developing capability by leveraging machine learning and computer vision, Pearl’s AI received FDA clearance for its clinical dental pathology detection in March 2022. It is currently cleared for clinical use in over 100 countries worldwide. Tanz says AI is now ready for customer adoption. “Because all this groundwork is laid, we are now in this position to get this capability deployed widely and [affect] billions of lives in a realistic way,” Tanz says.
Overjet's artificial intelligence analyzes radiographs in seconds, quantifying bone level measurements and detecting decay and calculus.
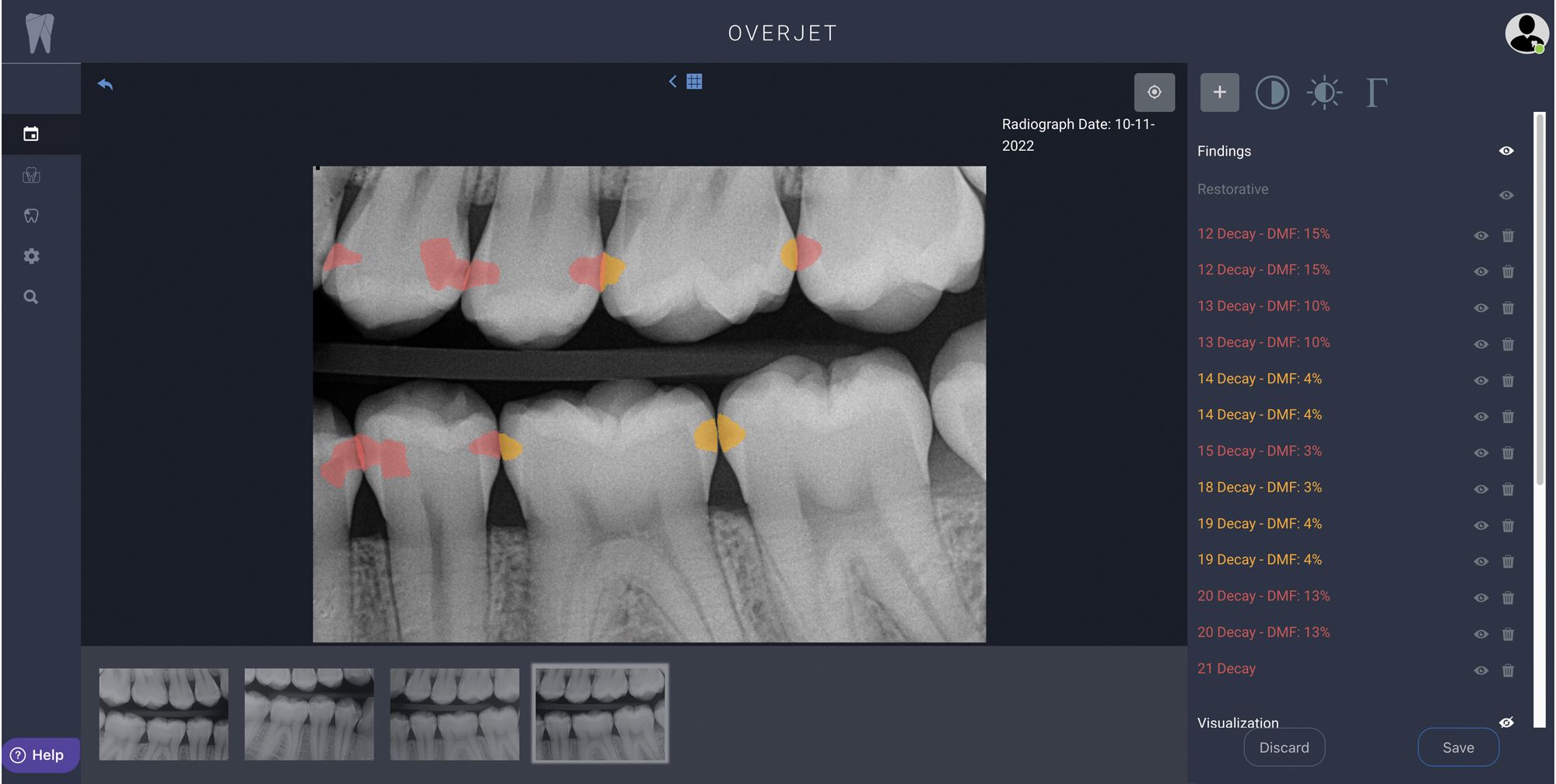
Wardah Inam, PhD, CEO and cofounder of Overjet, agrees that AI proves its value in dentistry every single day. It processes vast amounts of data in seconds, looking for patterns and trends that may have gone unnoticed. She says Overjet’s AI not only analyzes x-rays in real time to detect decay and possible indicators of periodontal disease but also reviews radiographs taken from prior visits and pulls in data from the practice management system (PMS) to help doctors with their clinical decision-making.
“It’s objective, not subjective, which standardizes quality of care and reduces the variations in diagnosis and treatment planning,” Dr Inam says. “The way Overjet’s AI displays the findings helps patients better understand their oral health. It builds trust and confidence in the doctor’s diagnosis, leads to more treatment acceptance, and leads to better patient outcomes.”
Like Overjet, Pearl’s AI also performs historical analysis and pulls data from PMS to provide insights that guide clinical decision-making. In addition to all the treatment benefits, Tanz explains that this functionality reinforces trust in patient relationships, an area of opportunity for many clinicians.
“There [are] already issues with patient trust in dentistry and wanting to get second and third opinions. [Patients] do inherently have some trust [in] computers by virtue of their interaction with that particular medium,” Tanz says.
“This is just the beginning,” Inam says, adding that analyzing and annotating x-rays to help with diagnostics and case presentation is only 1 area where AI can help. “AI applications will expand to analyze more data including 3D scans, intraoral images, and medical history. As dental and medical systems integrate, AI will play a critical role in predicting who may be at risk for oral disease and related health conditions. That will enable clinicians to take a more preventive approach in health care.”
Alex Sanders, PhD, CEO and cofounder of Diagnocat, says most practices are already doing digital dentistry. Implementing AI raises them to the next level. Diagnocat is the only AI that reads 3D cone beam computed tomography (CBCT) images, identifying over 65 conditions. In addition, Diagnocat 2D detects more than 35 dental conditions, which Dr Sanders says has a significant impact on improving the quality of diagnostics and the practical applications of digital dentistry.
“It analyzes CBCT, automates diagnosis and planning, and reduces the learning curve on expensive equipment,” Dr Sanders says. “Diagnocat 3D is AI for digital dentistry.”
Dr Sanders also says Diagnocat improves clinical consistency across team members and associates and is affordable, starting at $10 to $15 per day in many practices. “We sometimes forget our technical dental language is often lost on patients. Diagnocat provides an easy-to-understand visual report for you to review to help with case acceptance. Patients like the objectivity of the software, and you no longer have to be the bad guy delivering treatment plans,” Dr Sanders says. “The software does it for you.”
Inam says clinicians should experience AI to see how it will elevate patient care. Tanz agrees, adding that the technology has a low barrier for entry. All 3 CEOs have value propositions for clinicians. For example, Inam says Overjet is the only AI that is FDA-cleared for both detecting decay and quantifying bone levels, giving dentists information to use to determine restorative and periodontal treatment needs. Alternatively, Tanz highlights that Pearl AI is the only clinical AI cleared by the FDA for detecting 9 pathologic and restorative conditions on bitewing and periapical radiographs of permanent teeth for patients as young as 12 years.
Until you see what your patients’ x-rays look like with an AI overlay, Inam says it’s difficult to imagine how it will affect your practice. There’s a wow factor when clinicians see how easy it is to detect disease and show their patients the AI findings.
“With labor shortages and an uncertain economy, dentists and dental service organization (DSO) executives need tools that will streamline operations, save time, and increase treatment acceptance,” Inam explains. “I predict most dental practices will have AI for x-ray analysis within 5 years. AI analysis, electronic health records, online scheduling, [and] text to pay are just some of the ways technology is making dental practices more efficient.”
“It’s hard to find a good reason [to] not take advantage of the technology, especially [because] it’s so effective and affordable. AI software also accelerates the ROI for expensive CBCT equipment,” Dr Sanders states. “In addition, Diagnocat is an indispensable tool for DSOs and practice business managers who need to keep track of dental practice performance metrics such as turnover per primary patient.”
“It is amazingly accurate,” Tanz says. “I would encourage clinicians to try it out because it’s easy to set up and it’s a small investment, especially relative to the immense benefits it delivers to clinicians and patients. I’d rather them see for themselves vs take my word for it.”
Robotics in Dentistry
Robotics in dentistry is getting its start, according to Matthew Brignoni, business development manager of Zeeno Robotics. It’s so new that the state of robotics in dentistry today is comparable to where computers were in the 1980s.
Zeeno Robotics is starting with a few key functions to help practices show they are trailblazers in a wide-open future of robotics and dentistry. Zeeno, the first robotic office assistant of its kind, escorts patients, transports retainers and instruments, and even asks patients for a Google review.
Although it is forward-thinking, Brignoni says advancing technology should not come at the expense of humans delivering the patient experience. Instead, it should facilitate that experience. For example, if the escorted patient has dental anxiety or feels cold in the operatory, dental professionals should have time to grab a stuffed animal or blanket for the patient while the robot leads the patient back.
“With Zeeno, this robot escorts your patients, plays videos, and helps them fill out paperwork and so on, but someone’s controlling the robot. The robot is still bringing the patient to another human in the office, making that connection, and saving time so that human can elevate their patient experience while robots handle the repetitive things,” Brignoni says.
Brignoni says case studies are an excellent way for clinicians to educate themselves about technology. Another educational opportunity is a sales introductory call where you can ask questions about the product, which Zeeno Robotics calls the “discovery call.” “The biggest thing is to take that leap of faith,” Brignoni says. “You owe it to yourself to see [whether] the future of your practice has just arrived.”
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.