Careful planning, execution can get us closer to elusive perfection
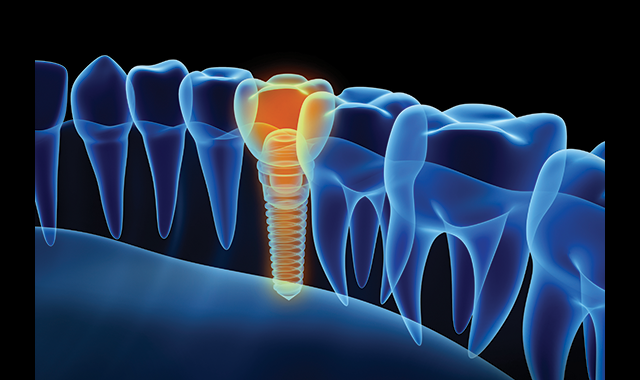
Continued development of imaging and instrumentation improves the predictability of implant cases.
Sometimes it’s hard to sleep when you are a practicing dentist. Anyone who has ever had the honor of having another human being place their health in “your” hands knows what I’m talking about. That person trusts that your expertise will give them an outcome that is as close to perfection as anyone can attain. That’s a lot of pressure and those of us in the profession know despite our very best efforts, things can still not go as perfectly as planned.
The thing about surgery (and for this discussion ALL dentistry is surgery) is sometimes you just don’t get a second chance. Now, that isn’t always the case. Things such as a crown with an open margin can be rectified by placing a new crown. However, there are many times and procedures in our profession where you quite simply will not get a second chance and those are the cases that keep dentists awake at night.
I’ll willingly admit I have had those nights where I lay in bed, watching the time pass on my ceiling projected clock, while I run through things over and over again in my mind wondering what I could have done differently. That type of reaction seems to be hard-wired into those of us who practice dentistry. We are trained and convinced that anything other than perfection is failure.
The bad news is perfection is truly unattainable. No matter how good we are and no matter how close we get, perfection, like infinity, is always just out of reach. The good news is advances in our profession are getting us exponentially closer to that goal.
Start a journal
One of the simplest ways to get better, in my opinion, is to monitor yourself. The old adage, “What gets measured gets improved” really is true. I’ve heard pilots are taught to evaluate each landing for both pluses and minuses. The idea behind that is to evaluate what went right so you can duplicate it and to evaluate what went wrong so you can improve it. I think that is incredibly helpful to dentistry as well.
Now I’m not advocating writing out several paragraphs about a successful buccal pit composite…unless you are really struggling with that procedure. Instead, I think when you start a very difficult, complicated, or multi-disciplinary case, it helps to sit down at the end of each appointment and evaluate the things that went well and the things that didn’t. This helps give you a more objective perspective and helps you improve for the next time.
Even if things go perfectly, thinking about the steps and writing them down can help solidify them in your mind for the next time.
One thing to remember from a technology perspective is if you are going to keep the journal in a digital format (and hey, why wouldn’t you?) make sure to do so in a HIPAA compliant manner.
Get access to a CBCT machine
Related Reading: A complete approach to implant planning
Ten years ago cone beam computed tomography was an incredibly expensive technology that existed primarily in learning institutions and the practices of specialists who dealt with extensive and complicated cases.
Fast forward to today and we are seeing market penetration of cone beam technology into many general practices. Part of the reason for this is the technology has become more affordable. However, more important than cost is the fact that more general dentists are placing implants. The use of CBCT in visualizing the surgical field is a tremendous asset.
I understand the investment required to bring CBCT into your practice is not a small one. Many practices that are just getting started have got to be cost-conscious, and there are also practices of doctors who are approaching the retirement phase of their practice and might not see the ROI of a substantial piece of equipment in the time left to practice.
In both of those scenarios, it may not be practical to invest in the technology. However, there is no rule that requires a practice to “own” the technology. Instead, I highly recommend you locate an outside source for CBCT scans. Many offices are willing to take scans for colleagues. There are also imaging centers and dental schools patients can be referred to.
Continue reading on the next page...
Utilize virtual treatment planning and surgical guides
One of the other tremendous advantages of 3D, in addition to being able to see the field in all three dimensions, is to treatment plan in 3D as well. The process is fairly straightforward.
The patient scan is opened in the 3D software and properly oriented. The implant type, length, and diameter is then selected. Once this step is done, a “virtual implant” will appear on the screen. It will look, for all intents and purposes, just like the real thing. The user can then “drag and drop” the implant around on the screen. The software allows the virtual implant to be oriented in any direction which means it can be placed into the placement site so it looks on the screen exactly as it will look when placed in the surgical site live. The implant can be moved up/down, left/right, and in/out until the user has the exact placement he or she would like.
More from Dr. Flucke: How expanding knowledge brings dentists new powers
At this point, the designed case can be saved in the same manner as saving any other computer file. The file is then sent to a lab in a HIPAA-secure manner and the lab will create a surgical guide that will allow for placement of the implant to the exact same parameters that were designed in the virtual treatment planning. Basically, if a second CBCT scan were taken after placement, the implant placement would be identical in both scans.
The surgical guide is self-limiting and only allows the placement to be in the same three dimensions as the treatment plan. Truly in cases of virtual treatment planning, the actual surgical placement is “the easy part” of the procedure. That is because all of the potential problems such as angulation, depth, avoidance of the inferior alveolar nerve, bone density, etc., have all been worked out in advance in the software.
For those doctors who are too busy or simply don’t want to have to learn this aspect of the process, there are laboratories who employ doctors to do this type of treatment planning as a service. The case is treatment planned and sent back to the referring doctor for their approval. Once the approval is received, the lab proceeds with the fabrication of the surgical guide.
Computer-controlled placement
Another piece of the puzzle to be solved can be solved by utilizing a “smart” handpiece. This is accomplished by using the iChiropro from Bien-Air. Implantology is a constantly changing science. As new and better designs are fabricated, these new and better designs require changes in surgical parameters.
Torque and RPM are both critical to surgical success and keeping abreast of changes to these requirements are intrinsic to that success. That’s where the intelligence of the iChiropro comes in.
The iChiropro is a surgical handpiece system that truly is “smart.” The system is controlled by an Apple iPad which runs an app created by Bien-Air. The app contains all of the settings for implants currently on the market. The user selects the implant and the app adjusts the handpiece for the proper RPM and torque - it’s that simple. Whenever an implant manufacturer announces changes to their parameters, those parameters are updated in the app which is then updated on the iPad.
The other “smart” part of the system is the ability to enter the patient’s name which allows the operator to have an exact record of the procedure for every patient.
Wrapping up
Implants are an amazing option to offer your patients. They are now so predictable I tell patients that if I was having a tooth extracted an implant would be my first choice as the replacement.
Yet, even as predictable as the procedure has become, it still needs to be carefully planned and executed. The good news is thanks to the continuing development of imaging and instrumentation the predictability continues to increase. While we may never quite get to “perfect” we continue to get closer and closer to that goal.
