6 mistakes dentists make placing implants
Implant failure is an outcome no one wants. Our experts share insight into common mistakes dentists make placing implants and what they can do to fix them.

No one wants an implant failure, but they happen nonetheless. There are many reasons that an implant fails, and they aren’t all the dentist’s fault. However, there are some common mistakes that dentists make placing implants that contribute to failure. We talked to implant experts to find out what these are and what you can do to avoid them in your practice.
All implants do not fail. Most of them succeed. Natalie Wong, DDS, Cert Prostho, FAAID, DABOI/ID, and the American Academy of Implant Dentistry (AAID) President, says they have one of the highest success rates in all of dentistry, even more successful than fillings.
“Our dental implant success rate is 90 to 95 percent at ten years,” Dr. Wong says. “I don’t think our fillings last that long.”
“In just about every situation, implant dentistry is the best way to replace a missing tooth or missing teeth for our patients,” agrees Adam Foleck, DDS, FAAID, DABOI/ID, and AAID Vice President. “It has the highest success rate of anything we are doing in dentistry, and because of that, it’s obviously one of the better choices for our patients.”
Dr. Wong says implants also feel the most natural, especially when compared to full and partial dentures or a bridge. Dr. Foleck agrees, adding that it is imperative to communicate these benefits to patients during treatment planning.
“Ultimately, we have to make sure that they understand the long-term benefit of a dental implant and how it can hopefully change their lives,” Dr. Foleck says.
Defining implant failure
These are, of course, the successful implants. However, what about the ones that do not succeed, the other five to ten percent? How do we ensure that we change patients’ lives for the better and not for the worse with a failing implant?
Per The Journal of Dental Implants, implant failure is caused by a multitude of factors, ranging from peri-implantitis, absence of osseointegration, and implant fracture. Also, surgical trauma, micromotion, and overloading can contribute to failure.
Failures are classified into two types, early and late failures. Early failures occur in the first three months after placement. Late failures happen after the first three months. These early and late failures are broken down further into different causal groups based on etiology, personnel responsible, failure mode, and biological causes.
Continue reading on the next page...
Early failures of implants:
- Etiology: Errors in implant selection, surgical placement, or restorative problems
- Personnel Responsible: Lack of expertise by dental professional or lab tech
- Failure Mode: Problems with osseointegration
- Biological Causes: The presence of peri-implantitis
Late failures of implants:
- Etiology: Patient’s other systemic conditions, lifestyle choices, or radiation treatments
- Personnel Responsible: Inadequate post-operative care by the patient
- Failure Mode: Either functional or physiological problems
- Biological Causes: Infection caused by peri-implantitis, traumatic occlusion, or overloading
Common mistakes dentists make placing implants
Many factors come together that lead to successful implants. Likewise, many things can go wrong that contribute to failure.
The dentist is only one part of the whole. However, he or she often has a significant influence on the success of the implant, either by case selection, implant therapy used, or experience with placement and surgery.
Our experts shared six common mistakes that dentists make placing implants. Best of all, they also shared how to avoid them.
Continue reading on the next page...
Mistake #1:
Not establishing adequate oral health and failing to adjust treatment plans for the bone available.
All implants need adequate bone and a healthy oral environment to have the best possible chance of success. Clark Damon, DDS, a private-practice dentist in the Amarillo and Dallas metro areas and a lecturer for Nobel Biocare and Neodent® for Straumann, says the most important thing to remember about implants is patients need to have bone and a healthy mouth to place an implant.
Should you be looking at a case where you have less than adequate bone or oral health, you need to adjust your strategy. Dr. Damon also encourages dentists to consider bone augmentation procedures either before the placement, or, in specific scenarios that allow it, at the time of placement.
“We need to ensure that the implant size selection is appropriate. In other words, we don’t want to choose a larger implant if we have less bone,” Dr. Damon says.
When Dr. Damon is placing permanent fixed teeth, most of his cases have a mouthful of periodontal disease. The high bacterial load intraorally can affect the opposing arch if there are implants, making it inadvisable to place an implant-retained prosthesis on either arch. In these cases, treating periodontal disease is crucial.
“That patient needs to be staged somehow, and both jaws need to be treated at the same time,” Dr. Damon explains. “Any time we are mixing teeth and implants, we must ensure that we treat the periodontal disease, ideally before the treatment, and then closely monitor the situation before we place implants.”
However, Dr. Damon clarifies eradicating the periodontal disease before placement is not as critical if all of the patient’s teeth are coming out. Full-arch implant therapy allows you more leeway in that respect.
Mistake #2:
Forgetting the fundamentals of occlusion with your freehand placement.
Raymond Choi, DDS, a mini-implant dentist and educator for Glidewell Laboratories, says when you improperly place an implant, it is not only tricky to restore, but it is also challenging for the patient to keep it clean in long-term maintenance. Moreover, implants that do not have a proper placement have problems in biomechanics and occlusion.

“Even if you can restore the tooth with the improperly placed implant, it’s not going to be a solid situation where heavy occlusal forces will be well received,” Dr. Choi explains. “You could have a restorative failure, screw loosening, and all of these things we don’t want to have.”
Improperly placed implants interfere with the fundamentals of occlusion. When you bite down, the forces from the occlusion transmit through the axis of the natural tooth.
When you replace a natural tooth with an implant, the angle of the implant should be the same so those occlusal forces then transmit through the axis of the implant.
“When the occlusal forces come in, and that force can be transmitted to the axis of the implant, then everything’s great,” Dr. Choi explains. “You are not going to see restorative complication.”
However, when the implant is not aligned with the axis of occlusal forces, then you start seeing screw loosening and breakage, among other things. These problems are challenging to resolve.
Dr. Choi says he has made this mistake many times over the last 25 years that he has been placing implants freehand. Today, it is much easier to get a proper placement with guided-surgery.
When you freehand placing implants, Dr. Choi says, you think you are on track for perfect placement. Then, after completion, you see you could have angled the implant differently. Guided implant surgery takes the guesswork out of the equation.
“Using surgical guides based on Cone Beam CT technology will prevent all these angling problems and improperly positioned implant issues,” according to Dr. Choi.
Continue reading on the next page...
Mistake #3:
Not starting with the tooth in mind
Dr. Wong says when looking at treatment options, dentists should, “start with the tooth in mind.” Many dentists focus on the bone first instead. That is because the surgical element of implant placement can be daunting to the patient and even the dentist, the focus tends to go there, Dr. Wong says.
“People are anxious about the surgery, so they spend a lot of time looking at the bone and planning on how to put the implant into the best bone. But, it may not be the best place for the tooth. Later on, we’re backtracking to figure out how to get it to work,” Dr. Wong explains.
Dr. Wong says the opposite should be the case. The implant should be prosthetically driven instead of surgically driven.
“We have to know where the tooth goes first, and then you put the implant in a position that can support that tooth,” she says. “Sometimes it goes in the existing bone. Sometimes we have to modify the bone to be able to get the implant into a restorable position.”
Dentists should plan the case from the tooth down, and when unable to get 1.5 mm of bone around the implant in the planning stage, they should consider using bone graft materials.
Starting with the tooth in mind means determining first where the tooth belongs in the bite and the jaw. Then, once you have established where the tooth needs to be, see if there is enough bone to put the implant where it needs to go for the tooth to line up in the surrounding dentition.
“Because sometimes we have a lot of bone, it’s just at the wrong angle,” Dr. Wong says.
When the implant is at the wrong angle, you can sometimes use angled abutments or screw channels to help correct it. However, Dr. Wong explains that these prosthetic parts can only correct angulation problems under 30 degrees. Once you get over 30 degrees off the optimal angle, the angled abutments can break during use because the angle is too severe. Another side effect of having the wrong angle is that the screw loosens.
“At the end of the day, you have to put the tooth where the tooth belongs,” Dr. Wong says. “I tell patients it’s like the Leaning Tower of Pisa. It just keeps leaning. They keep restoring it, but, over the long-term, it’s not going to work. It just keeps falling over.”
Part of the reason Dr. Wong supports the prosthetic approach first and starting with the tooth in mind is because bone grafting techniques are predictable today. If the bone isn’t perfect where you need it to be, you can enhance it with a graft.
“I would agree with you that 10, 20 years ago, our grafting wasn’t that good. We had to think about the bone first and not the tooth. Today we don’t need to do that anymore,” Dr. Wong explains.
Mistake #4:
Engaging in shallow placements
Dr. Damon says many times he thinks doctors have placements that are too shallow, which does not leave enough restorative space and does not allow for a proper emergence profile.
Emergence profiles have significant effects on the success of the implant. Each emergence profile is different based on the patient for whom you perform the restoration, but it should serve as a smooth transition from the implant platform to the natural shape of the patient’s tooth. Perhaps most importantly, it helps prevent “food traps” from forming around the restoration. A proper emergence profile allows the patient to maintain proper hygiene, without which the implant will fail.
The Whip Mix VeriGuide OS is a Class I, CE certified resin material developed for the production of high precision surgical guides for use in dental implant surgery.

However, in the mandible, Dr. Damon says, the depth to which you can place an implant is limited by the nerve. His workaround is to use a shorter implant that you drill down deeper to secure into the bone without hitting the nerve.
Another contributor to emergence profile problems is choosing an implant that is too small. Three clinical factors contribute to the emergence profile that a dentist should consider.
These include the thickness of the gingival tissue where you are going to place the implant, the size of the horizontal cross-section of the crown at the gum line, and the position of the crown comparatively to the bone.
When you choose an implant that is too small in the molar region, Dr. Damon says it can interfere with the emergence profile along the gum line. To combat this effect, Dr. Damon likes to use wide-platform implants in the posterior.
“I can get a nice, wide emergence profile,” Dr. Damon says. “Implant selection there is important.”
Dr. Damon keeps around 300 implants in stock so he can adapt to situations on the fly, if necessary. However, he says that having 30 implants (at a minimum) on hand or ordering multiple implants for a case allows you to give patients an excellent service.
Continue reading on the next page...
Mistake #5:
Not taking advantage of CBCT technology for treatment planning
When it comes to treatment planning, dentists today have many tools at their fingertips to help them get comprehensive data so they can strategize efficiently. Dr. Foleck is particularly enthusiastic about Cone Beam Computed Tomography (CBCT) technology for treatment planning.
“Hopefully, at this point in time, most people who are placing implants are using it,” Dr. Foleck says.
The advantages of CBCT technology are numerous, from the three-dimensional images they create to the details they provide that regular radiography doesn’t capture. CBCT also allows the dentist to create STL files or virtual teeth so they can place implants in an ideal space.
“The occlusion is incredibly important. Once the implant is placed surgically, failures long-term tend to be because of the patient not taking care of it or occlusal loading that is not ideal for the placement of the implant,” Dr. Foleck says.
SMOP from Swissmeda allows dentists and dental technicians to plan implant cases based on Cone Beam or CT data and to obtain precise drilling templates for use during implant placement.

The CBCT allows you to get a detailed look at the boney structures and dentition. However, it can’t show you everything. To ensure you have all the information you need, dentists should also get a sense of the overall health of the mouth.
Dr. Foleck advises dentists to use the CBCT scan for the planning, but also to take other factors into account. Determine whether the mouth has rampant periodontal disease which needs to be treated or whether the teeth above or below the implant have super-erupted, which would mean you need to place the implant deeper to accommodate for them. Also, look for keratinized soft tissue present that needs a tissue graft.
“The CBCT is great for showing us the bone, but to show us everything else that’s necessary, we need to take a look at the patient’s entire mouth,” Dr. Foleck says.
Mistake #6:
Not getting a tension-free closure during bone augmentation
Dr. Damon also says dentists should plan the case from the tooth down. Moreover, if you can’t get 1.5 mm of bone around your implant in the planning stage, you should consider bone augmentation.
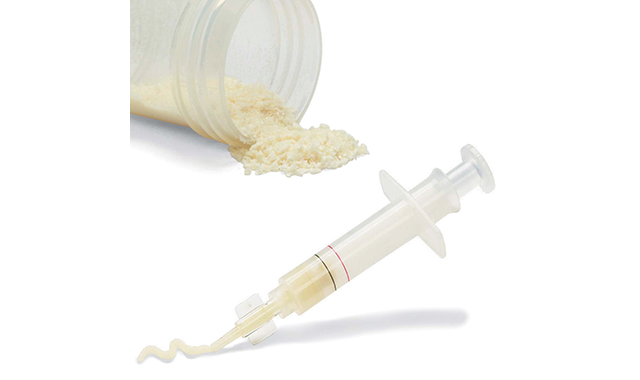
If you want to augment bone at the time of placement, you can do that in some instances, Dr. Damon says, but the bone needs blood. To allow for this, he suggests making cortical perforations. Also, when you are adding a particulate type of bone graft for single-implant placement, you need to cover it with a membrane, and it needs to stay sutured closed, as well.
“Since we are adding bone volume, you need to relieve tension on the flap,” Dr. Damon says. “They need to score the periosteum so that you get a tension-free closure.”
Dr. Damon says getting a tension-free closure is challenging for many dentists during bone grafting. However, when you score the periosteum, he says, you can pull up the flap and there’s no tension on it when you suture it closed.
The second most crucial point when bone grafting is to have a secured membrane to prevent fibrous encapsulation of the graft, Dr. Damon says. He is a fan of the sling-suture technique to secure the membrane when adding bone volume to the buccal surface of the bone.
“The options are to use tacks or screws or utilize the sling suture technique. I use that 80 percent of the time,” Dr. Damon says.
Continue reading on the next page...
What You Should Do Concerning Implants in Your Practice
Implant dentistry is enjoying excellent results. However, it is also a comprehensive restorative procedure. Implant dentistry requires knowledge of prosthetics and surgery, two complex areas by themselves.
For some dentists, placing implants can be intriguing but intimidating at the same time.
Dr. Choi, whose primary training course covers the basics of implantology, understands and has experienced these feelings firsthand. He recommends embracing the learning curve and doing as many implants as you can to get comfortable with it.
“It doesn’t help you if you only do one implant a month. You’ll never get over that learning curve. So, to become more comfortable with placing implants, you have to place a lot more of them,” Dr. Choi says.
Dentists wanting to get better at implants should get aggressive about doing more cases, he says. When he was starting, he gave significant discounts to specific patients to gain the experience he needed. Dr. Choi also encourages more education relevant to implantology.
“Every time you learn something new, that will add to your confidence level,” Dr. Choi says. “You’ll become more and more comfortable placing implants as you become more confident.”
Dr. Damon, who teaches an All-on-4 cadaver course, advises dentists to keep it simple at first. Start by finding a case where a healthy patient needs a single, posterior implant placement placed on a healed ridge.
“So, you extracted the tooth five months prior, and now the ridge is healed,” Dr. Damon says. “Place that implant. Choose that patient.”
Dr. Foleck also lectures and runs implant programs. He encourages dentists to take continuum courses that include placing implants on a model, a pig jaw, or a cadaver.
“It doesn’t have to be a live surgery right away. I think that intimidates some people,” Dr. Foleck says.
Dr. Foleck reminds dentists that implant dentistry is a commitment, and it needs a robust curriculum to address the surgical, prosthetic, and healing components of implant dentistry.
Also, the science of implant dentistry is different than it is with a natural tooth. Moreover, understanding the biomechanical and pharmacologic factors involved, as well as the physics and forces in loading, is crucial.
“It’s so important to take a course that addresses a lot of things. It’s not just about going in and placing an implant. There’s a lot of didactic information that is extremely important and also helps you to determine your next group of courses,” Dr. Foleck says.
Dr. Foleck says there are also great weekend courses, but he thinks those should follow the comprehensive courses. Weekend courses then supplement what you learned and build your skills. He also encourages mentorship programs with a local doctor who can come into your office and work with you directly.
“When you’re doing these programs, it’s important to do something that’s going to be inclusive of all stages of dentistry instead of just doing a surgical procedure or a bunch of surgeries,” Dr. Foleck says.
You can streamline implant treatments with the help of products such as the Dentsply Sirona Astra Tech Azento implant solution that puts the implant, surgical guide, restoration and related components in a convenient package.

Dr. Wong agrees, adding she thinks weekend courses tend to give you an introduction, and dentists who want more confidence with implant dentistry need more than that. Although it can be expensive, she thinks quality education is worth the price tag. She also supports the idea of mentoring with a credentialed dentist in implant dentistry.
“If you mentor under someone, you get their personal experience, which you often don’t even get out of a course,” Dr. Wong says. “In a course, they teach you the basics. They give you the science and fundamentals, but usually in overall, general terms.”
Dr. Wong also encourages dentists to pursue a credential from the AAID. It requires preparation, experience, and presenting cases for peer review, but it helps with confidence.
“What makes our credential different is that we expect you to be knowledgeable in both the surgery and the restorative aspects. You have to defend both, and for our highest level, our Diplomate, you have to defend both at a specialist level,” Dr. Wong says. “I would agree that our exam is challenging, which is what makes it valuable and worthwhile. It is a credential, once earned, to be proud of.”
Dr. Choi also emphasizes you cannot ever stop learning about implants. With all the of the fields involved, ranging from biology to physiology to occlusion and TMJ, to name a few, implant dentistry asks the dentist to be an expert in many disciplines. Plus, there are many new technological advances implant dentists must keep up with that change how implants are done, as well.
“Dentists must commit himself or herself to continue to learn more and more. Implant placement is not something that you can just do after taking a couple of weekend courses,” Dr. Choi says. “Anyone can drill a hole in the bone and put a screw in there, but implantology is a lot more than that.”

ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.
Product Bites – November 10, 2023
November 10th 2023The weekly new products podcast from Dental Products Report is back. With a quick look at all of the newest dental product launches, Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Amann Girrbach, DMG, Pac-Dent, and ASI Dental Specialties. [4 Minutes]