Vital Pulp Therapy in Mature Permanent Teeth: A Paradigm Shift
It’s important to understand this treatment modality and its challenges.
Vital Pulp Therapy in Mature Permanent Teeth: A Paradigm Shift. Image courtesy of destina/stock.adobe.com.
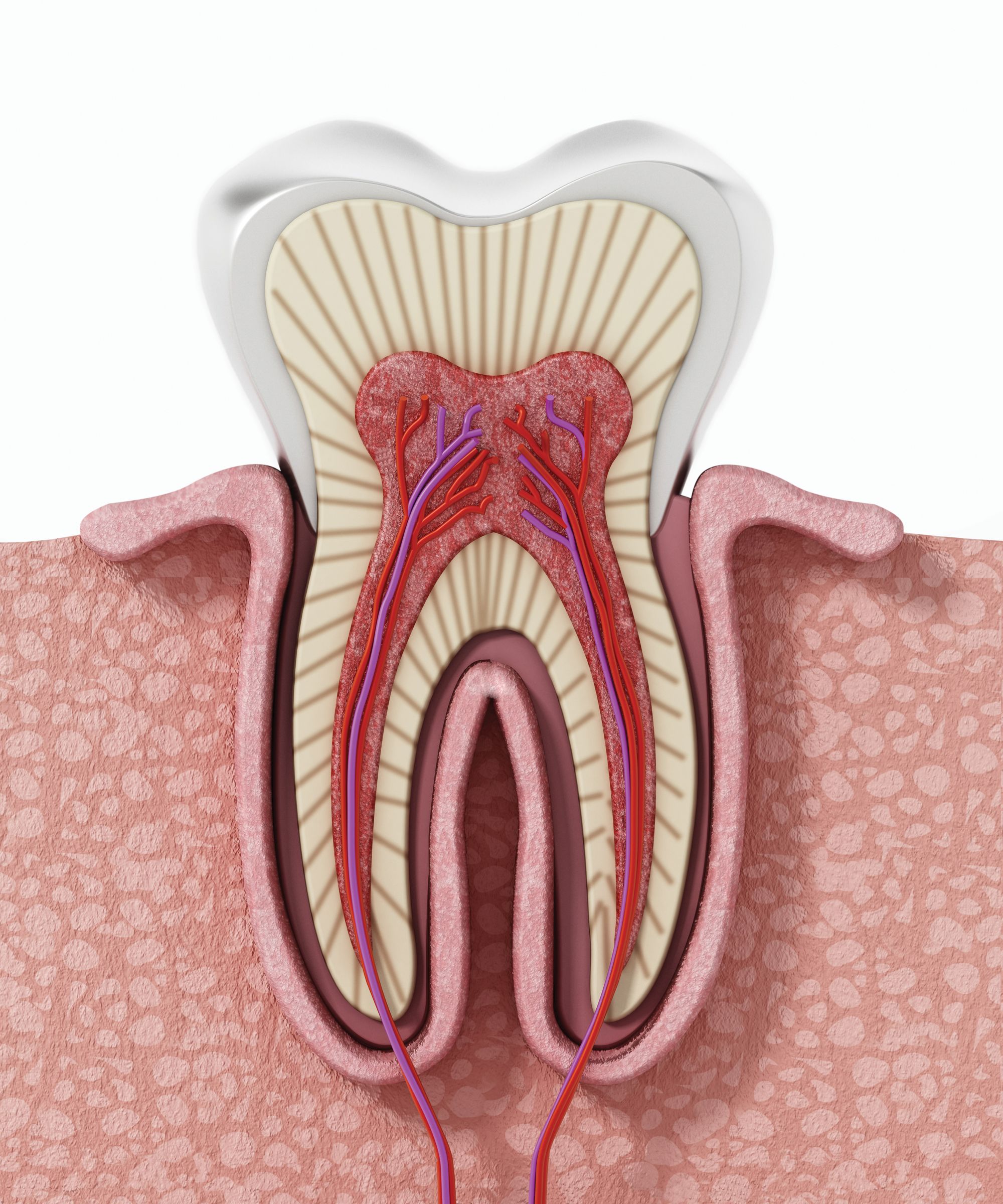
The spectrum of procedures from pulp capping to pulpotomies, known as vital pulp therapy, has been a mainstay treatment modality to manage deep caries in the primary dentition and immature permanent dentition. In the latter, vital pulp therapy is employed to facilitate root development, otherwise known as apexogenesis. Traditional materials for vital pulp therapy included formocresol and calcium hydroxide. Although treatment with these materials was associated with reasonable success in these primary and immature permanent teeth, success was less predictable in mature permanent teeth.1-4
This difference in prognosis stems from the anatomic differences in pulp tissue that occur secondary to root maturation. The robust vasculature and stem cell populations found in immature roots allow them to regenerate even under unfavorable conditions, whereas mature permanent teeth possess more limited mechanisms to survive pulpal irritants.5 Mature permanent teeth with carious pulp exposures were given a diagnosis of “asymptomatic irreversible pulpitis” because that carious pulp exposure was thought to induce terminal pulpal inflammation.6 The historic treatment recommendation for teeth with asymptomatic irreversible pulpitis was nonsurgical root canal therapy, with its increased risk of complications including root fracture as well as increased restorative needs over the lifetime of the tooth.7-9
The introduction of bioceramics, a class of calcium silicate-based materials with distinct biocompatibility advantages, has shifted this paradigm and calls into question the diagnosis of asymptomatic irreversible pulpitis. According to the new position statement from the American Association of Endodontists, vital pulp therapy with bioceramics now represents the treatment of choice for certain carious exposures in mature permanent teeth.10-12 Large-scale studies showcase the ability of bioceramics to repair carious exposures and reverse early-stage pulpal irritation for these teeth. Furthermore, success rates for vital pulp therapy with bioceramic materials are comparable to those for nonsurgical root canal therapy.1,7,13,14
Figure 1A

Figure 1B
Figure 1C. Preoperative images (A and B) depicting deep caries in tooth No. 2 without associated symptoms or clinical testing abnormalities allowed for conservative direct pulp capping to manage the carious exposure (C).
Bioceramic materials aren’t exclusive to vital pulp therapy. They are mainstay repair materials for root canal perforations and have been widely utilized as retrofilling materials during apical microsurgery. This is in large part due to their favorable interactions with cells from the periodontal ligament and alveolar bone, promoting bone regeneration in a way that other dental materials are incapable of doing.15 Further research on their interaction with pulp tissues has highlighted their unique potential in vital pulp therapy. Bioceramics are nonirritating to pulpal tissues and provide an excellent seal against microbial contaminants.16 Their placement adjacent to the pulp tissue promotes pulp survival. Their mechanism of action is similar to calcium hydroxide in contact with the pulp. They create a localized area of tissue necrosis, followed by calcific bridging. Their enhanced coronal seal is thought responsible for their markedly higher success rates as direct pulp-capping agents.1,15,17
The improved outcomes in vital pulp therapy are attributable to bioceramics, although several other treatment-related factors have a demonstrable positive impact on outcomes.10 These include careful disinfection, minimization of additional pulpal irritation, and magnification. Careful disinfection includes the use of dental dam isolation, clean water supplies, and irrigation of the pulp exposure with sodium hypochlorite. Avoiding microbial contaminants is necessary because microbes are a known pulpal irritant. Clinicians must also be mindful of minimizing additional pulpal irritation, particularly by employing water coolant spray when removing caries adjacent to the pulp. High temperatures are known to produce pulpal necrosis. Lastly, magnification is known to enhance outcomes. Magnification, via the surgical operating microscope or loupes, is essential for accurate visualization of pulp tissues as well as complete caries excavation.
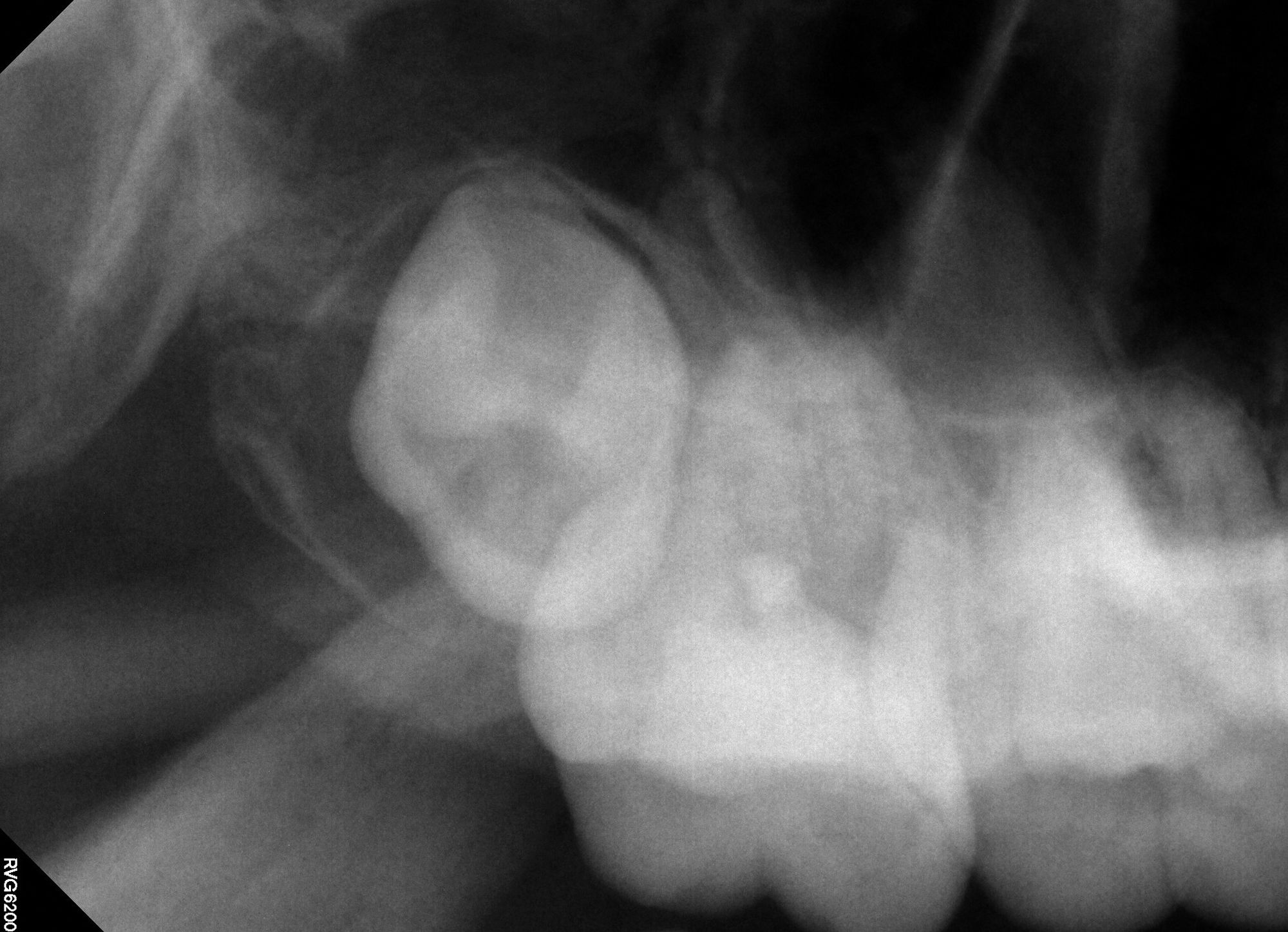
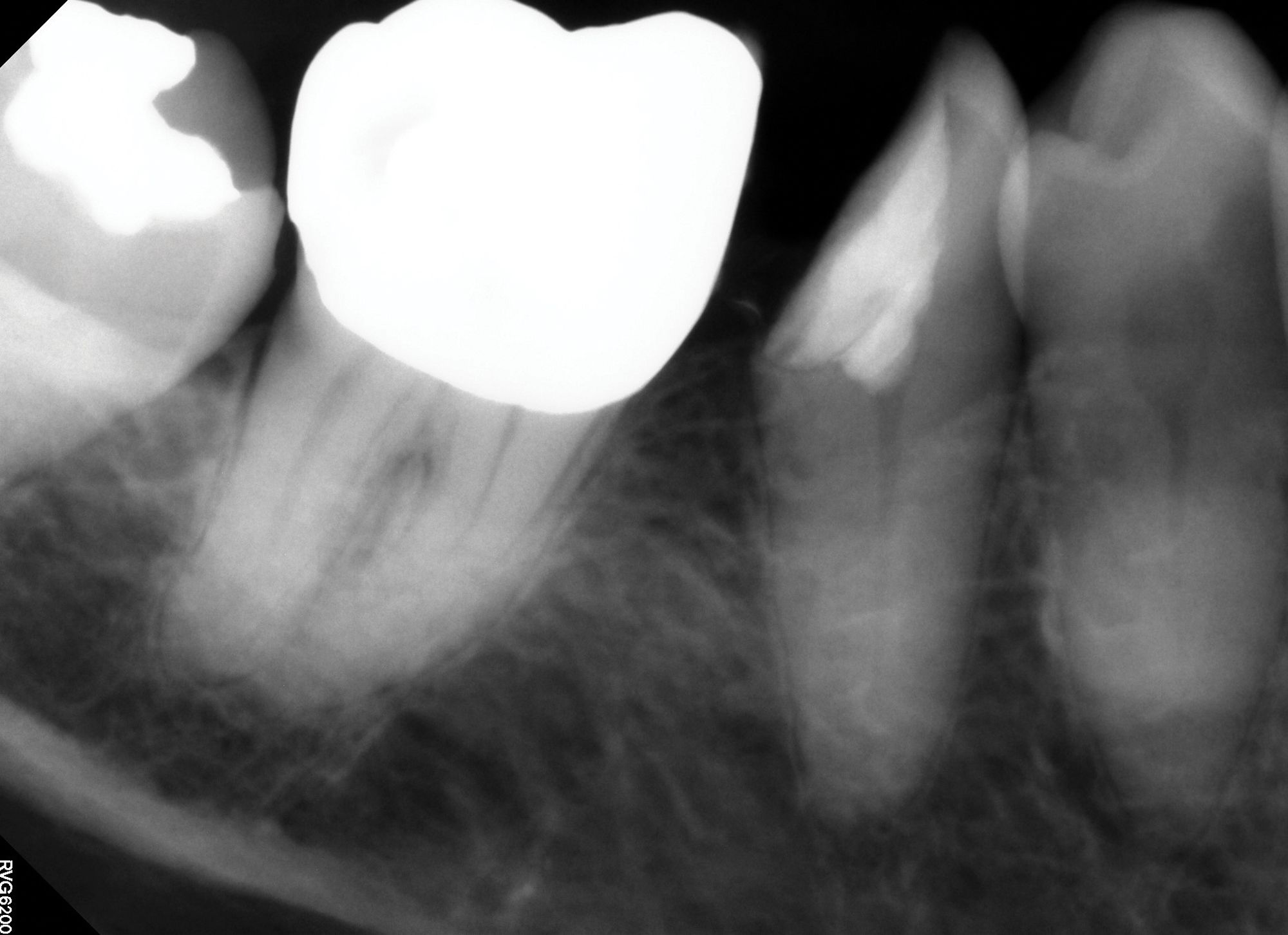
Figure 2A
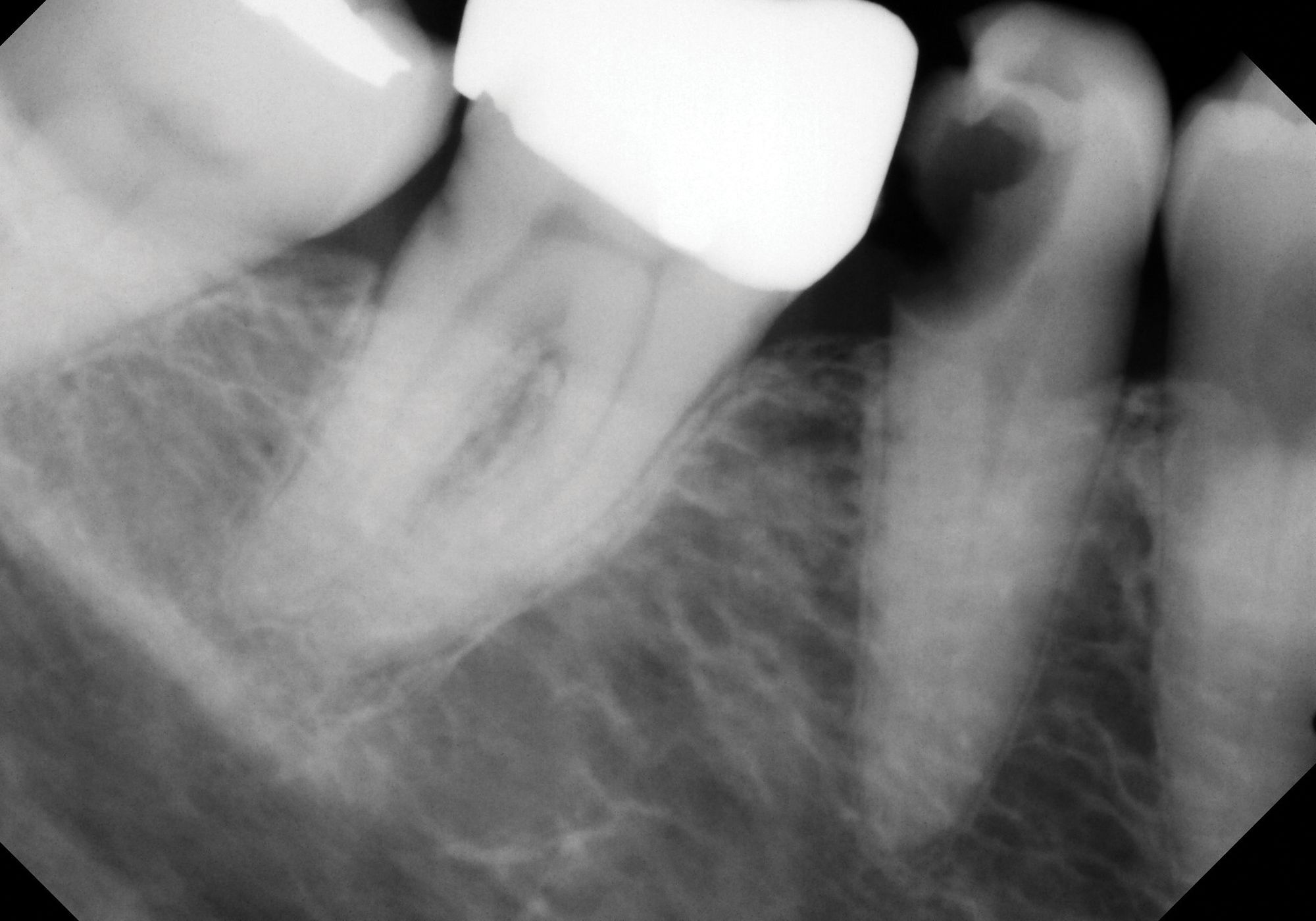
Figure 2B. Deep caries associated with signs and symptoms of reversible pulpitis in tooth No. 29 (A) resulted in hyperemic pulp tissue extending throughout the pulp chamber, warranting bioceramic pulpotomy to achieve hemostasis (B).
The recommendation to treat mature permanent teeth with carious pulp exposures with vital pulp therapy techniques represents a paradigm shift in endodontics.
Diagnosis and Treatment Planning
Careful diagnosis and case selection are foundational to the appropriate provision of vital pulp therapy. In mature permanent teeth with carious pulp exposures, the health of the pulp tissue must be ascertained prior to selecting vital pulp therapy as the treatment of choice. A confirmed response to pulp sensitivity testing must be obtained, and cold testing is considered the most reliable means of testing.18 Baseline testing of control teeth can indicate the reliability of testing in the individual patient. Although some patients may not experience a cold response, including older patients with dentinal tubules or pulp chambers that have undergone calcification, many individuals who warrant consideration for vital pulp therapy will have viable and robust pulps that will respond to this test under normal circumstances.19 That said, when in doubt, electric pulp testing can serve as a viable sensitivity test alternative. Patients should, however, be made aware of limitations in pulp sensitivity testing potentially creating false negatives.18
Pulp sensitivity tests are used to establish the pulpal diagnosis.6 Teeth with a diagnosis of normal pulp, indicated by a normal response to cold, or those with a diagnosis of reversible pulpitis, a hypersensitive but not lingering response to cold, can in most cases be appropriately treated with vital pulp therapy. Teeth with a diagnosis of irreversible pulpitis, namely a hypersensitive and lingering response to cold, may also be treated by vital pulp therapy in certain circumstances. Data support the application of bioceramic-based vital pulp therapy ranging from direct pulp caps to pulpotomy, even in exposed pulps with evidence of pulpitis.13,14 These data have many discussing potential changes to the diagnostic terminology of asymptomatic irreversible pulpitis. Wolters et al proposed a new classification system dividing irreversible pulpitis into initial, mild, moderate, and severe iterations to better classify treatability using minimally invasive methodologies.20
Most agree that teeth with evidence of progressive irreversible pulpitis, in which degeneration of the pulp is imminent, should be treated more aggressively given the high likelihood of microbial contaminants and progression to apical periodontitis. Therefore, spontaneous or unprovoked pain and percussion tenderness indicative of apical periodontitis are considered contraindications for vital pulp therapy and indications for pulpectomy instead.21 Teeth with a diagnosis of pulp necrosis are also not candidates for vital pulp therapy.
Figure 3A.

Figure 3B. Although vital pulp therapy was planned for tooth No. 31 during the consultation visit—at which the patient had no symptoms or abnormalities on clinical testing (A) —discomfort and cold sensitivity on the day of treatment were consistent with hyperemic pulp tissue extending into the roots. The diagnosis of symptomatic irreversible pulpitis instead warranted nonsurgical root canal therapy to manage (B)

Treatment plans for vital pulp therapy fall on a spectrum, depending on the extent of inflammation visualized during care. Updated protocols for the use of bioceramics should still be applied to primary and immature permanent teeth. However, the novel applications discussed include certain mature permanent teeth with carious or traumatic exposures. Direct pulp capping with bioceramics should now be considered primary treatment for asymptomatic carious exposures, with few exceptions. Partial or full pulpotomies may be required when there is evidence of additional inflammation.10
Ultimately, the choice to pursue vital pulp therapy versus nonsurgical endodontics involves a thoughtful and comprehensive approach to treatment planning. In many cases, the benefits of minimally invasive care offered by vital pulp therapy permit more conservative restorative care. This reduces risks of postoperative complications secondary to tooth structure removal, including fracture. More conservative restorative care also is associated with a reduced cost.21
Pursuing vital pulp therapy does not obviate the future development in some patients of pulpal or periapical disease warranting endodontic interventions. In certain cases, this risk of future treatment needs may be intolerable, such as when major restorative procedures are indicated that could be compromised by a future endodontic access. For example, a tooth that is planned to serve as a fixed partial denture abutment, in which the inherent risk of future endodontic involvement is high and access through the occlusal surface risks the integrity of the new restoration, might be considered for nonsurgical root canal therapy over vital pulp therapy even in the absence of symptoms.22 Similarly, patients with certain medical comorbidities, such as patients with poorly controlled diabetes, may have a higher risk of progressive apical periodontitis and reduced success with treatment, so a thoughtful discussion may warrant more aggressive endodontic interventions in an earlier stage for the individual.23,24
Treatment Protocol
Comprehensive informed consent should precede the delivery of all dental care, including vital pulp therapy, and both verbal and written consent is advisable. Patients must be informed about the potential for treatment progression depending on clinical findings. This means that during treatment, patients should be aware that signs of pulpal inflammation may warrant progression from planned direct pulp capping to partial or full pulpotomy or even pulpectomy.
If pulp necrosis is indeed found upon caries excavation, the provider must have already obtained informed consent for pulpectomy. For example, although many teeth undergoing vital pulp therapy may be definitively restored using direct composites, indirect restorations involving full cuspal coverage are warranted when pulpal disease necessitates pulpectomy on a posterior tooth.25,26 Postoperatively, patients should understand that signs or symptoms of pulpal disease may progress and therefore may require greater levels of endodontic intervention. Follow-up and awareness of the potential downstream need for nonsurgical root canal therapy should be a part of the informed consent process.
Following consent, the patient should be comfortably anesthetized. Adequate anesthesia should be confirmed by a negative cold test on the tooth to be treated. Dental dam isolation must be applied, and clinicians must confirm the absence of saliva contamination or leakage.10 Although single tooth isolation is traditionally employed for endodontics, involvement of interproximal surfaces in many vital pulp therapy cases necessitates multiple tooth or quadrant isolation. Disinfection of the coronal surface can be considered to eliminate superficial contaminants prior to caries removal. This can be accomplished with sodium hypochlorite or hydrogen peroxide rinses.
Caries should be excavated with a high-speed handpiece with sufficient water coolant spray to minimize overheating of the pulp, with direct effects to reduce caries vitality in the present and future.10 Although this is the standard set forth by Occupational Safety and Health Administration, it bears repeating that dental water lines must be free of bacteria because minimizing contamination is essential for vital pulp therapy. Even though protocols for indirect pulp capping sometimes advise leaving caries to avoid pulp exposure, the use of bioceramics warrants complete caries excavation to eliminate sources of microbial recontamination.10,11 Complete caries excavation should be confirmed visually with magnification, tactically by contact with sound, as well as with the use of caries detecting agents or laser fluorescence.10
Caries removal in these cases will result in pulp exposure. Hemostasis of a vital, bleeding pulp may be achieved with the use of sodium hypochlorite as a rinsing agent or with pressure applied via a soaked cotton pellet.10 Sodium hypochlorite possesses superior efficacy and safety versus other hemostatic agents, including epinephrine or ferric sulfate.21 Clinicians should, however, be prepared for cases in which hemostasis is not immediately achievable.10 Continued bleeding indicates more extensive inflammation with an expected lower success of vital pulp therapy due to persistent postoperative inflammation. Furthermore, bleeding is associated with poorer sealing of the bioceramic materials, wherein microbial recontamination will impede healing. In these cases, additional pulp tissue should be removed with the high-speed handpiece under water coolant or a sterile spoon excavator.16 The partial or full pulpotomy should be completed up to the level so that hemostasis can be readily achieved. If hemostasis remains unachievable, pulpectomy should be initiated.10
Once hemostasis is achieved, exposed pulp tissue should be dried and restored with a 1- to 2-mm thickness of bioceramic material. Several bioceramic options are available in the dental marketplace. It behooves any clinician to understand the benefits of each before choosing which to utilize. Early iterations of mineral trioxide aggregate (MTA) were associated with significant dental staining. Their use should therefore be limited, especially in esthetic zones in favor of nonstaining alternatives.27,28
Additionally, many practitioners find MTA challenging to handle and prefer newer putty-based bioceramic materials. Of note, resin-containing calcium silicate materials should not be utilized for vital pulp therapy procedures given the cytotoxic effects of resin-based materials on the dental pulp.21 Bioceramics are more costly than prior materials used in vital pulp therapy. However, cost-effectiveness analysis finds that they, in fact, represent more economical options given their higher success and reduced lifetime need for retreatment.29
Following placement of the bioceramic plug, the tooth may be immediately and definitively restored.
Conclusion
The advent of bioceramic materials has ushered in a paradigm shift in endodontics. Nonsurgical root canal therapy is no longer the standard recommendation for an asymptomatic or mildly symptomatic carious pulp exposure. Ultimately, clinicians should be prepared for the potential need for vital pulp therapy during any restorative procedure in which the possibility of pulp exposure exists. The pulp tissues of mature permanent teeth are exquisitely sensitive to pulpal irritants in the form of restorative materials, especially resin-based materials; thus, their use should be absolutely avoided when pulpal exposures occur. The routine use of dental dam isolation during restorative dentistry, especially when work approximates the pulp, and ready availability of simple materials including sodium hypochlorite and bioceramic cements can have a great impact on long-term pulpal health.
References
Kundzini R, Stangvaltaite L, Eriksen HM, Kerosuo E. Capping carious exposures in adults: a randomized controlled trial investigating mineral trioxide aggregate versus calcium hydroxide. Int Endod J. 2017;50(10):924-932. doi:10.1111/iej.12719
Langeland K. Management of the inflamed pulp associated with deep carious lesion. J Endod. 1981;7(4):169-181. doi:10.1016/S0099-2399(81)80231-2
Mjör IA. Pulp-dentin biology in restorative dentistry. part 7: the exposed pulp. Quintessence Int. 2002;33(2):113-135.
Tronstad L, Mjör IA. Capping of the inflamed pulp. Oral Surg Oral Med Oral Pathol. 1972;34(3):477-485. doi:10.1016/0030-4220(72)90327-1
Kling M, Cvek M, Mejare I. Rate and predictability of pulp revascularization in therapeutically reimplanted permanent incisors. Endod Dent Traumatol. 1986;2(3):83-89. doi:10.1111/j.1600-9657.1986.tb00132.x
Glossary of endodontic terms. American Association of Endodontists. May 7, 2020. Accessed August 3, 2022. https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/
Awawdeh L, Hemaidat K, Al-Omari W. Higher maximal occlusal bite force in endodontically treated teeth versus vital contralateral counterparts. J Endod. 2017;43(6):871-875. doi:10.1016/j.joen.2016.12.028
Caplan DJ, Cai J, Yin G, White BA. Root canal filled versus non-root canal filled teeth: a retrospective comparison of survival times. J Public Health Dent. 2005;65(2):90-96. doi:10.1111/j.1752-7325.2005.tb02792.x
Fuss Z, Lustig J, Katz A, Tamse A. An evaluation of endodontically treated vertical root fractured teeth: impact of operative procedures. J Endod. 2001;27(1):46-48. doi:10.1097/00004770-200101000-00017
Clinical guidelines position statements. American Association of Endodontists. March 14, 2022. Accessed August 3, 2022. https://www.aae.org/specialty/clinical-resources/guidelines-position-statements/
Bjørndal L, Simon S, Tomson PL, Duncan HF. Management of deep caries and the exposed pulp. Int Endod J. 2019;52(7):949-973. doi:10.1111/iej.13128
Li Z, Cao L, Fan M, Xu Q. Direct pulp capping with calcium hydroxide or mineral trioxide aggregate: a meta-analysis. J Endod. 2015;41(9):1412-1417. doi:10.1016/j.joen.2015.04.012
Asgary S, Eghbal MJ. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: a multi-center randomized controlled trial. Acta Odontol Scand. 2013;71(1):130-136. doi:10.3109/00016357.2011.654251
Asgary S, Eghbal MJ, Bagheban AA. Long-term outcomes of pulpotomy in permanent teeth with irreversible pulpitis: a multi-center randomized controlled trial. Am J Dent. 2017;30(3):151-155.
Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review--part II: leakage and biocompatibility investigations. J Endod. 2010;36(2):190-202. doi:10.1016/j.joen.2009.09.010
Hilton TJ. Keys to clinical success with pulp capping: a review of the literature. Oper Dent. 2009;34(5):615-625. doi:10.2341/09-132-0
Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--part I: chemical, physical, and antibacterial properties. J Endod. 2010;36(1):16-27.doi:10.1016/j.joen.2009.09.006
Mainkar A, Kim SG. Diagnostic accuracy of 5 dental pulp tests: a systematic review and meta-analysis. J Endod. 2018;44(5):694-702. doi:10.1016/j.joen.2018.01.021
Ketterl W. Age-induced changes in the teeth and their attachment apparatus. Int Dent J. 1983;33(3):262-271.
Wolters WJ, Duncan HF, Tomson PL, et al. Minimally invasive endodontics: a new diagnostic system for assessing pulpitis and subsequent treatment needs. Int Endod J. 2017;50(9):825-829. doi:10.1111/iej.12793
Hargreaves KM, Berman LH, Rotstein I, Cohen S. Cohen’s Pathways of the Pulp. 12th ed. Elsevier; 2021.
Cheung GS, Lai SC, Ng RP. Fate of vital pulps beneath a metal-ceramic crown or a bridge retainer. Int Endod J. 2005;38(8):521-530.doi:10.1111/j.1365-2591.2005.00982.x
Aminoshariae A, Kulild JC, Mickel A, Fouad AF. Association between systemic diseases and endodontic outcome: a systematic review. J Endod. 2017;43(4):514-519. doi:10.1016/j.joen.2016.11.008
Marotta PS, Fontes TV, Armada L, Lima KC, Rôças IN, Siqueira JF Jr. Type 2 diabetes mellitus and the prevalence of apical periodontitis and endodontic treatment in an adult Brazilian population. J Endod. 2012;38(3):297-300. doi:10.1016/j.joen.2011.11.001
Sorensen JA, Martinoff JT. Intracoronal reinforcement and coronal coverage: a study of endodontically treated teeth. J Prosthet Dent. 1984;51(6):780-784. doi:10.1016/0022-3913(84)90376-7
Suksaphar W, Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y. Survival rates from fracture of endodontically treated premolars restored with full-coverage crowns or direct resin composite restorations: a retrospective study. J Endod. 2018;44(2):233-238. doi:10.1016/j.joen.2017.09.013
Beatty H, Svec T. Quantifying coronal tooth discoloration caused by Biodentine and EndoSequence root repair material. J Endod. 2015;41(12):2036-2039. doi:10.1016/j.joen.2015.08.032
Vallés M, Roig M, Duran-Sindreu F, Martínez S, Mercadé M. Color stability of teeth restored with Biodentine: a 6-month in vitro study. J Endod. 2015;41(7):1157-1160. doi:10.1016/j.joen.2015.03.014
Schwendicke F, Brouwer F, Stolpe M. Calcium hydroxide versus mineral trioxide aggregate for direct pulp capping: a cost-effectiveness analysis. J Endod. 2015;41(12):1969-1974. doi:10.1016/j.joen.2015.08.019