Spotting the trouble: Successful endodontic treatment
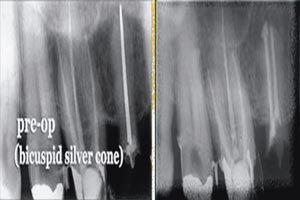
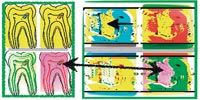
FIGS. 1–2 Radiographs showing an endodontic case that required retreatment (Fig. 1, above). Radiographic evidence colored to highlight the discovery of anomalous pulp stones (Fig. 2, below).
THE SET-UP“It has long been a bias of mine that what takes place before the root canal is started goes a long way to determining the quality of the end result. Dr. Jeffrey Linden has written a clinically relevant and concise piece to address many of the key concepts needed to guide the delivery of top level endodontic care.”-Dr. Richard E. Mounce, team lead
With any treatment protocol, dentists must achieve two concurrent objectives. They must deliver the highest standards of patient care, while at the same time-using the latest technological advances in dentistry-they must ensure treatments are accomplished efficiently and painlessly at a reasonable cost.
Fortunately, these two objectives are, more often than not, complementary. Maintaining high care standards is often far less costly, in both the long- and short-term, than treatment performed to lower standards. When viable bacteria remain in the root canal there is a risk of periapical infection. Many endodontic failures can be attributed to coronal leakage resulting from failed restorations. With the high frequency of apical periodontitis, the science reports retreatment including restoration and prosthetic replacement has hada huge economic cost of billions of dollars.
Diagnostics: Foundation of endodontic success
Root canal therapy most likely will be successful if the canal is free of infection when obturated. The optimal approach is an accurate diagnosis to instrumentation strategies thoroughly removing tissue and shaping the coronal midroot and apex. The goals of root-canal therapy involve treating pulpal bacterial infection by removing infected tissues within the chamber, thorough cleansing mirroring the individual root anatomy and effectively sealing the tooth to prevent re-infection (Fig. 1). Careful diagnosis and cleaning of the tooth improves the long-term success rate of endodontic procedures and, at the same time, reduces the chances retreatment will be necessary.
Current negative pressure irrigation techniques such as the Endovac and thorough apical instrumentation with a system such as Lightspeed LSX, from Discus Dental (discusdental.com), are among the latest cleaning and shaping instruments. Additionally, the corded gutta-percha system, Obtura III Max from Obtura Spartan (obtura.com), and the cordless Hotshot from Discus make obturation easier and complete.
In today’s endodontic practice, we identify a number of techniques and therapies that improve practice efficiency and healing rate, either by enhancing outcomes, streamlining procedures, or both. Endodontists may disagree about the best way to fill root canals, but there is no dispute that the key to endodontic success is the complete removal of the microbes.
Identifying periapical pathosis and its management requires a complete clinical and radiographic exam. Apical periodontitis is inflammation of the surrounding tissues and the surrounding dentin at the root system’s portals of entry. Therefore, understanding the extent of the infection along with the overall structural soundness of the tooth is critical to ensuring the procedure will be both efficient and successful.
Endodontic imaging
Interpretation of a radiographic image is subjective and a learned skill regardless of the radiographic options we have today. Diagnosticians use oral x-rays and now innovative Cone Bean Computed Tomography (CBCT) systems as part of their armamentarium. But regardless of the imaging technology used, the epiphany comes from the diagnosis the image makes available and not the image itself.
Radiographs are a two dimensional view of a three dimensional phenomenon inconsistently showing changes of the clinical and biologic conditions. Off-angled films can enhance the diagnostic assessment of root canals including traumatic injuries, coronal, horizontal, and at times, vertical root fractures. Deviations on the mineralization and structure of the bone adjacent to the affected area enable us to potentially visualize calcifications and resorption.
Cutting edge digital radiography is basic for diagnosis and treatment. The addition of DEXIS’ new Platinum Sensor and its ability to generate 16,000 shades of gray in 2.2 megapixel radiograph images provides for sharper image quality for visualization on a large monitor.
Anatomic anomalies and variations in the root canal shapes and space and occasionally pulp stones (Fig. 2) are identifiable on radiographs and CBCT scans. That said, canals are infrequently as straight as they may appear on a radiograph. They tend to be oval and irregular rather than round and regular, and typically present with a variety of curvatures, including deltas and bayonet shapes (Fig. 3) making instrumentation more challenging. An additional mesiobuccal canal is seen in Fig. 4, a mesial-angled radiograph of a mandibular molar with 5 canals.
Of course obtaining these images can be difficult, especially when a rubber dam in place in the patient’s mouth (noncompliance is not an option), makes positioning of the film or sensor even more challenging.

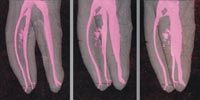
FIGs. 3–4 The roots on this radiograph have been colored to highlight the variety of irregular canal anatomies that are commonly found (Fig. 3, above). Teeth-such as this one with five-can have unusual numbers of canals. (Fig. 4, below).
Other diagnostics
In addition to x-rays, there are several other diagnostic tests to identify the nature and extent of the bacterial infection. Vital pulp tests are essential components of the endodontic consultation. The hot and cold test, pulp vitality test (to check for failing pulpal blood circulation, not vitality), percussion, palpation for sensitivity and evidence of breakdown are all key in differentiating diagnoses.
In the process of making a diagnosis, an important step is to reproduce the symptoms of the patient’s chief complaint. This should be clearly explained to the patient for accuracy. The patient should understand in advance what to expect from the tests to maximize the value of the information obtained.
It should be emphasized that once pulp is stimulated with cold, there is a refractory period before a second cold or a hot test can be accurately conducted. More often, most endodontic tests are comparative tests; contralateral teeth and neighboring teeth should be tested for the contrasting normal responses. These vital pulp testing strategies enable the patient to appreciate the normal pulpal responses exhibited by asymptomatic teeth. Repeated testing reduces the probability of false positives or negatives.
For trauma cases, obtaining films taken prior to the injury is critical to proper diagnosis to gauge the progressive sizes of the lesion and provide appropriate treatment planning. In trauma and carious exposure cases in young patients with immature apices, the extent of the pulpal involvement and apical closure is of primary consideration. In cases where immature apices are affected, drug therapy with calcium hydroxide or mineral trioxide aggregate (MTA) can help promote apexification.
By obtaining a thorough diagnosis, endodontic procedures can be performed with as clear a treatment plan as possible, helping to reduce the incidence of surprises that may add time to a procedure. Therefore, a systemic approach to diagnostic judgment is key to prevent misinterpretation and mistakes. As stated by Dr. Richard E. Mounce, “Most of the clinical issues and challenges that bedevil treatment are foreseeable.”
With endodontics, the most efficient procedure is the procedure that is well planned and executed from the start. By properly diagnosing the condition of the tooth structures and thoroughly removing as much infected material as possible, the practitioner ensures the procedure will go smoothly with treatment to the highest standard. Success rates will be high-and that’s a strong foundation for any dental practice.

Dr. Jeffrey W. Linden is assistant clinical professor, Columbia School of Dental and Oral Surgery, Attending, St. Barnabas Hospital/Cornell Medical Center. An international lecturer on ultrasonic endondontics, Dr. Linden maintains a private practice in endodontics and endodontic surgery in New York City. He can be reached by calling 212-595-1161, or online at endonyc.com or jefflinden@earthlink.net.
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.