How to use new materials and workflows to restore edentulous patients
Finding the right materials to create a simplified restorative workflow for predoctoral dental students.

Patients with edentulous arches are prevalent in today’s society. But with the advent of implants, more patients are able to have similar form and function to what they were previously accustomed. Within our dental program, we wanted to find a material and system that would allow optimal outcomes and allow our predoctoral students to complete cases from start to finish.
Complete edentulism is a multifactorial concern for a patient’s physical and psychological health. Our patients’ chief complaints with total edentulism and the available prostheses are the following: loss of taste; difficulty chewing efficiently; maintaining stability and adherence to soft tissue and bony structures; speech concerns; texture of prosthesis; size of prosthesis; and periodic sore spots.
Three biomimetic and biocompatible materials recently entered the marketplace. They’re all millable and permit composite resins or milled crowns to be bonded to the substructures. The three materials are TRINIA™, from Shofu, Trilor® from Bioloren, and Pekkton® Ivory from Cendres+Métaux Medtech. These high-performing polymers all vary slightly in makeup and composition. TRINIA and Trilor are fiber-reinforced.
TRINIA is the product we’ve been testing. Unlike bone, it’s isotropic, meaning mechanical properties, including strength, are similar in all directions. We’ll review in vitro findings and several clinical cases that used this new material.
Related reading: The evolution of dental materials
Finding the right materials
It’s estimated 30 percent of adults over the age of 65 are edentulous, especially in underserved communities.1 Edentulous patients wanting a fixed hybrid type of prosthesis present to our clinic on a regular basis. These cases can be very complex in a graduate program but can be insurmountable in a predoctoral program.
We set out to find an implant system and restorative material suited for faculty guided predoctoral procedures.2-4 Because of the patient pool’s concern for metal allergy, we were also looking for a metal-free option.5,6 In dealing with edentulous maxilla and mandibles, there’s a wide array of treatment options to consider.7-12 Our goal was to stay away from complicated procedures such as bone augmentation or distraction osteogenesis.
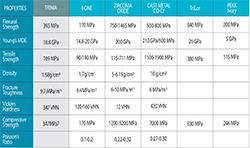
Short implants have had very good success rates13,14 and could reduce the restorative complexity for our students. In addition, the material for the prosthesis needed to be forgiving, reparable and relatively easy to seat in the mouth.15,16 The combined Bicon SHORT® implant system and the TRINIA fiber-reinforced hybrid resin material showed great promise as a solution.15-22 Before placing the fiber-reinforced composite substructures in patients, we performed in vitro studies to determine the material’s flexural strength and flexural modulus. We compared those to zirconia and cast metals.23,24
Related reading: Digital advances alter the denture landscape
Having a flexural modulus similar to bone25-29 would be advantageous in that it would allow the two systems to work in synergy and preserve bone support30-33 around the implants while reducing post placement chipping and fractures of teeth and the substructure. A second concern was the material should have a density similar to bone in order to help the patient have a more natural feeling, as if they had their own dentition.
Previous patient retrospective studies found some patients didn’t like the bulkiness of the fixed hybrid prosthesis and the resulting time-consuming maintenance needed to retain proper oral hygiene.12
Continued on page two...
Material tests
TRINIA blocks were obtained from commercially available stock, and a Beuhler IsoMet™ 5000 slow speed rotary diamond linear precision saw was used to cut 0.25 mm thick samples from the block in directions parallel to, perpendicular to, and 45º to the long axis of a TRINIA block. Samples were placed into dimethyl sulfoxide (DMSO) solvent for 30 days, sputter-coated with gold, and imaged in a scanning electron microscope (SEM). Fiber orientation and the interaction between fiber and polymer were photographed (Figs. 1-2).
Fig.1
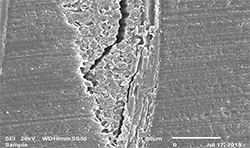
Fig.2
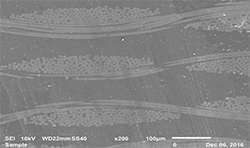
Fig.1
To measure the flexural strength of TRINIA, blocks were cut into micro-tensile bars following ISO 4049. The resulting bars were individually measured using an electronic digital caliper. 25 Specimens of TRINIA with final dimensions of 2 x 2 x 25 mm (+/- 0.1 mm) were made without regard to orientation of the cut within the block. Specimens were stored in reverse osmosis (RO) water at 23o C for 24 hours before flexure testing. A universal testing machine was used to perform 4-point-bend testing (crosshead speed = 0.5 mm/min). Flexure strength and flexural modulus were reported. Data was analyzed using two factor ANOVA along with post-hoc tests (Table 1).
TRINIA displayed densely packed perpendicular bundles of interwoven fibers. These bundles ran continuously in both directions regardless of the orientation of the sample cut.
The following case studies demonstrate an example of a difficult restorative case for a predoctoral dental student made simpler with available products and techniques. We found Bicon SHORT Implants and TRINIA metal-free substructures are a strong combination when used for completely edentulous patients.
Patient 1
A 71-year-old male presented with a full maxillary denture and retained lower left canine and lower right first premolar (Fig. 3). He desired a semi-permanent solution to improve fit, function of upper and replace all missing teeth on the lower. An initial panoramic radiograph was taken for surgical and restorative planning purposes. The patient and doctor discussed options and it was decided a new maxillary full denture and a fixed hybrid prosthesis on the lower arch would be acceptable treatment options.
Fig.3

Fig.4
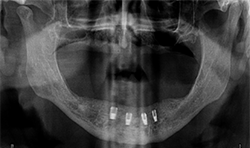
Fig.3
Continue to page three...
The patient’s medical history was evaluated for a mandibular fixed hybrid prosthesis using four Bicon implants and a TRINIA substructure. A CBCT revealed adequate bone for implantation and reviewed clinically after properly dissecting the mental nerve to avoid paresthesia. Four implants were placed through the anterior to increase the AP spread. Mandibular full thickness mucoperiosteal flap across the ridge was released and mental foramen were identified bilaterally. The posterior implant was placed 5 mm anterior to the mental foramen. All sites were prepared, checked for parallelism and enlarged to receive four implants each 4 mm x 8 mm with a 2.5 well (Fig. 4).
After normal healing and integration, 5 x 5 mm healing abutments with 2.5 mm wells were placed. At the impression appointment, the sulcus was prepared using a sulcus reamer and a PVS impression was taken and sent to the lab. The patient was happy with the wax try-in and the lab was instructed to finish the case. Delivery was uneventful (Figs. 5, 6).
Fig.5

Fig.6

Fig.5
At the one-month, post-op appointment the patient reported being able to eat corn on the cob and was happy with the fit and function of his hybrid, and the prosthesis continued to perform properly at subsequent follow-up visits.
Patient 2
A 69-year-old male presented with an existing maxillary full denture and mandibular fixed partial denture (Tooth Nos. 22-27) with pain and suppuration on abutment teeth supporting the FPD (Figs. 7, 8). All existing abutment teeth were carious and periodontally involved. It was decided with the patient the best treatment option would be to extract the remaining mandibular teeth. All options were presented to patient and patient desired a fixed hybrid for both arches.
Fig.7

Fig.8

Fig.7
Continue to page four...
All dental records were taken including a CBCT which revealed inadequate bone height for traditional implant lengths. The decision was made to use four Bicon SHORT implants with a TRINIA framework and Ceramage teeth from Shofu.
Surgical guides were fabricated using Anatomage software. A maxillary sinus lift was performed on the upper right and left quadrant areas using a lateral sinus window approach. Bone grafts were placed with 50/50 allograft and xenograft with a PRF membrane. After normal healing time all remaining mandibular teeth were atraumatically removed and socket preservation performed using non-demineralized bone grafting material and CollaTape. The patient was fitted with interim full dentures on both arches.
Healing occurred without incident and an appointment was made for implant placement. The maxillary arch received two 5 x 6 mm, one 3.5 x 8 mm and two 4 x 8 mm Bicon SHORT Implants during the first implant placement appointment. The implant in the upper left area was placed as a precaution against the possible loss of one in the premolar area. All Maxillary implants successfully integrated.
Fig.9

Fig.10

Fig.9
At a second appointment, four Bicon SHORT implants, three 4 x 6 mm and one 3.5 x 8 mm were placed in the mandibular arch (Figs. 9, 10). After normal healing time, both the maxillary and mandibular arches were fitted with a fixed hybrid prosthesis fabricated from a TRINIA substructure and Ceramage denture teeth. The patient was happy with the fit, function and comfort (Fig. 11).
Fig.11

Conclusion
The previous case studies demonstrate difficult restorative cases made easier with the products and techniques now available. Using Bicon SHORT Implants and TRINIA metal-free substructures in our predoctoral clinics has become a successful combination for completely edentulous patients.
TRINIA telescopic prosthetic material has revolutionized the ability for our predoctoral students and general practitioners to be successful with all-on-four semi-removable prosthetic appliances. This combination is a great option for patients who do not want any metal prostheses in their mouth, but want a semi-permanent restoration when edentulous. Many patients comment that their new fixed-hybrid feels very similar to their original teeth because they do not have the additional weight of a metal framework.12
Continued on page five...
This product has a lower flexural modulus than zirconia, and can be used with a greater distal cantilever on the prosthesis without undue torque or component failure. Having a material with a flexural modulus close to that of bone allows it to bend at relatively the same rate and helps to maintain healthy bone support around the implants; but more importantly this allows the patient to function similar to when they were dentate. TRINIA has high flexural and compressive strengths. It is also easily adjustable chairside and can be bonded for exact fit.
Using the Bicon implant system and telescoping crown abutments, the TRINIA base is a perfect match. Within the system of four implant copings, two are passive and two are retentive. The patients report the restorations feel natural, lightweight and chew and function similar to their natural dentition.
Our in-vitro findings demonstrated TRINIA could not only withstand the compressive and functional loads placed upon it during mastication, but it had a more favorable flexural modulus when compared to metal or zirconia materials.
Patient satisfaction has been noted to be highly positive to the use of these two materials as a system. Patients especially appreciate the similar density to bone, so there is a weightless feeling to the prosthesis similar to natural dentition.
Trending: How old is too old for overdentures?
One of the most important physical characteristics of TRINIA is in its isotropic mechanical properties. Deformation in the mouth is significantly reduced due to the interwoven glass fiber mesh contained in the resin matrix. The torque on the mandible is negligible because of the matched modulus. These two properties allow a greater distal extension on the substructure, which in turn allows for safer and more predicable implant for predoctoral dental students.
About the authors:
P. Bradford Smith, DDS, Dean
Dr. Smith graduated from Brigham Young University in 1983 with a B.S. in zoology. He attended the University of the Pacific School of Dentistry and graduated in 1986 with a D.D.S. degree. Dr. Smith was an Adjunct Professor/Clinical Instructor at the U.O.P. extramural clinic in Sacramento for two years. Dr. Smith moved to Sacramento, California where he practiced for 22 years before accepting a position as an Assistant Professor at Midwestern University College of Dental Medicine in July of 2008. He has worked in the Preclinical Sciences developing the curriculum since the inception of the program. He was asked to be the Preclinical Director of Oral Health Sciences in 2009 and the Assistant Dean for Preclinical Sciences in 2010, Associate Dean in 2011, and Dean in February 2015. Dr. Smith has research interests in dental materials, specifically ceramics, hybrid polymers and dental cements. He is also involved in digital dental solutions in patient care. Dr. Smith completed scholarly work at the Costin Institute and graduated as a Costin Scholar in September of 2010. He is a Fellow of the American College of Dentists, and International College of Dentists, and member of Omicron Kappa Upsilon National Dental Honor Society. He has served in the Lasers in Dentistry Special Interest Group with ADEA, and as the chair in 2015-16.
John C. Mitchell, PhD – Assistant Dean for Dental Research/Professor:
Dr. Mitchell earned his PhD from The Ohio State University in 1999, in the dual fields of Tissue Engineering & Implant Biomaterials Science. In 2001, he joined the Oregon Health & Science University as an Assistant Professor, holding appointments in Restorative Dentistry, Pediatric Dentistry, Biomedical Engineering, and in the School of Medicine. Tenured as an Associate Professor in 2006, he became Professor and Director of Research in 2012. Dr. Mitchell joined Midwestern in 2013 as the Director of Dental Biomaterials Research, and was tenured and promoted to Assistant Dean for Research in 2016. He has been the advisor/mentor for over 150 student and resident researchers, many of whom have won awards. He helped establish the MWU Dental Student Research Group and serves as their Faculty Advisor. Dr. Mitchell was named as the SCADA National Faculty Research Advisor of the Year for 2011, and the AADR/NSRG Faculty Mentor of the year in 2017. He was named as an AADR Fellow in 2016. Mitchell has received research grants totaling nearly $5 million, a United States Patent in 2012, and has several other patents pending. Amongst other awards, Dr. Mitchell received the Sigma Xi Outstanding Faculty Researcher Award, the Oregon BioSciences Innovation Award, and the IADR/GSK Innovation in Oral Health Care Award. Formerly the Associate Editor for Journal of Dentistry, Dr. Mitchell routinely reviews articles for several journals and also grant submissions to the NIH. He has been the President, Secretary & Treasurer, and Councilor for the Implant Research Group of the International Association for Dental Research, served as an Executive Board member of the American Association for Dental Research, and is currently the President & Founding Member of the Arizona Section of the AADR.
References
1. US Department of Health and Human Service, Oral health in America: A Report of the Surgeon General-Executive Summary. Rockville, Md: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research National Institutes of health. 2000
2. Springer. Design of Artificial Human joints and Organs. Pal, S. 2014, XX, 419 p 217 ISBN: 978-1-4614-6254-5 Ch. 2 Mechanical Properties of Biological Materials.
3. Malo p, De Arroyo Nobre M, Lopez A, et al. All-on-4 immediate function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long term (5 years) outcomes. Clin Implant Dent Relat Res. 2012;14 (Suppl 1) : e139- e150
4. Box VH, Sukotjo C. Patient-Reported and Clinical Outcomes of Implant-Supported Fixed Complete Dental Prostheses: A comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. Journal of Oral Implantology. 02/2018, Vol 44, Issue 1
5. Moffa JP. American Dental Association. Biological effects of nickel-containing dental alloys. Council on Dental Materials, Instruments and Equipment. J Am Dent Assoc 1982: 104: 501-505
6. Passaretti A, Petroni G, Miracolo G, et.al. Metal free, full arch, fixed prosthesis for edentulous mandible rehabilitation on four implants J of Prosth research April 2018 Vol62 Issue 2 264-267
7. Stumpel L, Haechler W. The Metal-Zirconia Implant Fixed Hybrid Full-Arch Prosthesis: An Alternative Technique for Fabrication. Compendium of Continuing Education in Dentistry. Mar2018, Vol.39 Iss 3, p176-181.
Conclusion on page six...
8. Malo P, Nobre M, Guedes C, et.al. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant –supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin Implant Dent Relat Res. 2018;1-11
9. Tiossi R, Gomes E, Faria A, et.al. Biomechanical behavior of titanium and zirconia frameworks for implant- supported full-arch fixed dental prosthesis. Clin Implant Dent Relat Res. 2017; 19:860-866
10. Kwon T, Bain P, Levin L, Systematic review of short-(5-10 years) and long-term (10 years or more) survival and success of full-arch fixed dental hybrid prostheses and supporting implants. Journal of Dentistry 42 (2014) 1228-1241.
11. Patel P. The Solid Zirconia Implant –Retained Prosthesis: An Excellent Full-Arch Alternative to the Fixed Hybrid Denture. Dentistry Today Oct 2015
12. Box V, Sukotio C, Knoemschild K, et al. Patient- Reported and Clinical outcomes of Implant-Supported Fixed Complete Dental Prostheses: A comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. Journal of Oral Implantology Feb. 2018, Vol 44, No. 1, pp. 51-61
13. Wagner F, Seemann R, Marincola M, Ewers R, Fixed, fiber-Reinforced Resin Bridges on 5.0mm Implants in Severely Atrophic Mandibles: up to 5 Years’ Follow-Up of a Prospective Cohort Study. Journal of Oral and Maxillofacial Surgery (2018), 10.1016/j.joms. 2018.02.001
14. Seemann, R. Marincola M, Seay D, et al. Preliminary Results of Fixed, Fiber-Reinforced Resin Bridges on Four 4.5 mm Ultrashort Implants in Compromised Bony Sites: a Pilot Study. Journal of oral and Maxillofacial Surgery, April 2015 Vol. 73, Issue 4, p. 630-640
15. Biris C, Bechir E, Bechir A, et al. Trinia Reinforced Polymer as Core for Implants Superstructure. J of Materiale Plastice 54; No. 4. 2017
16. Collis J. Crafting metal-free substructures using Shofu’s TRINIA for a new option in substructure work. Dental Lab Products 6/2015
17. Lombardo G, Pighi J, Marincola M. Cumulative Success Rate of Short and Ultrashort Implants Supporting Single Crowns in the Posterior Maxilla: A 3’
18. Bonfante E, Suzuki M, Carvalho R, et al. Digitally Produced Fiber-Reinforced Composite Substructures for Three-Unit Implant-Supported Fixed Dental Prostheses. The International Journal of Oral and Maxillofacial Implants, April 2015, p. 321-329
19. Ewers R, Marincola M, Perpetuini P, Morgan V, The Bicon Short Implant: A Thirty-Year Perspective Editor Morgan VJ, Quintessence Publication Co. Chicago 2017
20. Pohl, V., Thoma, D. S., Sproniak-Tutak, K, Garcia-Garcia, A. Short dental implants (6mm) versus long dental implants (11-15mm) in combination with sinus floor elevation procedures: 3-year results from a multicenter, randomized, controlled clinical trial. Journal of Clinical Periodontology 2017 Vol 44: 438-445.
21. Ghensi P, Tonetto G, Soldini C, Dental Implants with a platform-switched morse taper connection and an osteo growth induction surface. J Craniofac Surg. 2018 Nov 2 doi:10.1097/SCS0000000000004795. Epub ahead of print.
22. Ravida A, Wang IC, Barootchi S. Meta-analysis of Randomized Clinical Trails Comparing Clinical and Patient-Reported Outcomes Between Extra-Short (<6mm) and Longer >10mm) implants. J Clin Periodontal. 2018 Oct 25, doi:10.1111/jcpe.13026. Epub ahead of print
23. Odahara T, Matsumoto H, Chiba A, Mechanical Properties of Biomedical Co-33Cr-5Mo-0.3N Alloy at Elevated Temperatures. Materials Transactions, Vol. 49, No. 9 (2008) pp. 1963-1969
24. Altarawnew, S. Limmer, B. Reside G Dual Jaw Treatment of Edentulism using implant supported monolithic Zirconia fixed Prostheses. Journal of Esthetic & Restorative Dentistry March 1, 2015
25. Shahar R, Saslansky P, Barak M. et.al. Anisotropic Poisson’s ratio and compression modulus of cortical bone determined by speckle interferometry. J of Biomechanics 40 (2007) 252-264
26. Currey J, What Determines the Bending Strength of Compact Bone? The Journal of Experimental Biology 202, 2495-2503 (1999)
27. Silva M, Bone Mechanical Testing by Three-Point Bending. Washington University Musculosketal Structure and Strength Core. May 2016
28. Ruschel G, Gomes E. Mechanical Properties and Superficial Characterization of a milled CAD/CAM glass fiber post. J of Mechanical Behavior of Biomedical Materials Vol 82, June 2018, pgs. 187-192
29. Rho J, Ashman R, Turner C. Youngs Modulus of Trabecular and Cortical bone material: Ultrasonic and Microtensile Measurements. J of Biomechanics Vol 26, Issue 2, Feb 1993, pgs. 111-119
30. Jacobs R, Schotte A, van Steenberghe D, et al. Posterior jaw bone resorption in osseointegrated implant- supported overdentures. Clin Oral Implants Res. 1992:3:63-70
31. Karl M, Taylor TD. Bone adaptation induced by non-passively fitting implant superstructures: a randomized clinical trial. Int J Oral Maxillofacial Implants 2016;31(2): 369-375
32. Van Eijden, T.M.G.J. Biomechanics of the Mandible. Crit Rev Oral Biol Med 11(I):123-136 (2000)
33. Tassani S, Homan C, Baruffaldi F Volume to density relation in adult human bone tissue. J Biomech. 2011 Jan 4:44(1): 103-8.
34. Manicone P, Iommetti P, Raffaelli L, An Overview of zirconia ceramics: Basic properties and clinical applications. Journal of Dentistry 35 (2007) 819-826
35. Keyoung Jin, Jong Yeop Lee Comparative study of mechanical properties of dental restorative materials and dental hard tissues in compressive loads. J Dent Biomech.2014; 5:1758736014555246
36. Soares PB, Nunes SA, Franco SD, Measurement of elastic modulus and Vickers hardness of surround bone implant using dynamic microindentation-parameters definition Braz Dent J. 2014 Sep-Oct;25(5):385-90
37. CoorsTek amazing solutions, formerly Dynamic Ceramic; precision engineering. www.dynacer.com/data-sheets/zirconia/
38. American Elements; The Advanced Materials Manufacturer. www.americanelements.com/cobalt-chromium-alloy

ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.