Fighting Recurrent Decay with Your Materials and Techniques
A significant cause of restoration failure is recurrent decay. Can today's materials and techniques help prevent it?
Fighting Recurrent Decay with Your Materials and Techniques.
Photo courtesy of Aleksandra Gigowska/stock.adobe.com.
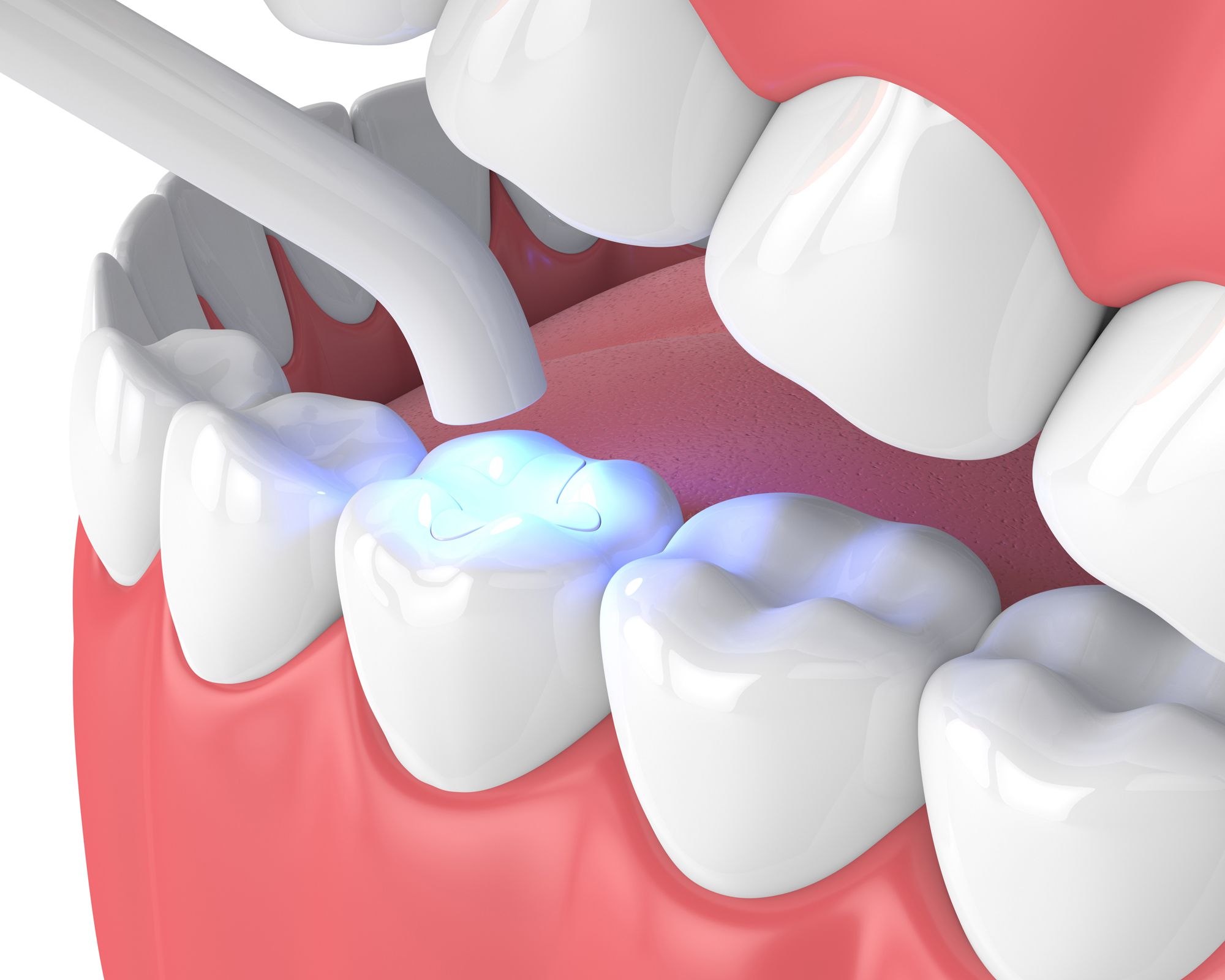
Recurrent decay is a significant cause of restorative failure. However, both innovative and established materials and protocols can help prevent it.
Recurrent decay occurs under existing restorations and is a primary reason for restorative replacement. Even the best materials and techniques cannot eliminate the risk of it. The best defenses are consistent oral health care with fluoride, along with regular cleanings and dental visits, and preventing micro-crack formations.1 These leakage pathways allow acids and bacteria to get into the restoration and out of oral hygiene tools' reach, causing decay and, possibly, restorative failure over time.2
While some contributors to recurrent decay are outside clinical control, like poor oral hygiene, other risks of it dentists can minimize, like the development of microscopic pathways for leakage. Let's look at how today's materials and attention to proven techniques can help prevent recurrent caries.
New Materials to Defend Against Recurrent Decay
For many years, materials manufacturers have been combating recurrent caries with materials. Nathaniel Lawson, DMD, PhD, Division Director of Division of Biomaterials at the University of Alabama at Birmingham School of Dentistry, says any material that releases ions present in tooth structure seems to help prevent demineralization of surrounding tooth structure in laboratory studies.
"Another method to prevent recurrent decay would be to create a material to which bacteria cannot attach. That's the idea behind some new experimental materials," Dr Lawson says.
Manufacturers have attempted to prevent recurrent decay with materials in a few ways. There were fluoride-releasing resin materials that used various methods to instigate the delivery—from using ion exchanges in the patient's oral fluids to incorporating the properties into the monomers—which manufacturers introduced over the past few decades.
In 2018, researchers and engineers in Canada proposed adding filling materials with self-assembling antimicrobials into dental composite resins. These fillers were made of antibacterial drugs and silica glass organized at a molecular level that supplied the properties of the material for years.3
The following year, researchers in Israel suggested incorporating a modified amino acid molecule, fluorenylmethylloxycarboyl (Fmoc)-pentafluoro-L-phenylalanine, which had antimicrobial properties and self-assembly at the nanoscale.4
Infinix™ from Nobio has a lineup of advanced antimicrobial restorative materials designed to prevent recurrent decay. The line uses Nobio's patented QASi antimicrobial particle technology. In addition, their product line includes an antimicrobial bonding agent and the first FDA-cleared antimicrobial composite.
Although he has not tested the material himself, Dr Lawson says the idea behind Infinix is it contains quaternary ammonium compounds, which have an electric charge. The electric charge works to break the cell walls of bacteria that want to stick to the surface of the composite. He says that the best demonstration he saw involved putting Infinix and another composite into a well and curing it. Then, after adding saliva and a growth medium, incubating the wells for 24 hours and checking the pH to see what happened.
"You can check to see that the pH of the competitor composite has dropped to around 4 while the Infinix composite is still around 7.5. This shows that Infinix could potentially kill bacteria so that it cannot metabolize the growth medium, produce lactic acid, and lower the pH," Dr Lawson says.
Troy Schmedding, DDS, AAACD, recognizes and appreciates the trend for bioactive and antimicrobial materials for restorative dentistry and sees the benefit of using adhesive materials with a history of fighting recurrent decay.
"Kuraray has a tradition and foundation in restorative dentistry that is tried and true," Dr Schmedding says.
The chemistry of materials can also prevent recurrent decay in the restoration, Dr Schmedding says, particularly in adhesive systems. For example, Kuraray's MDP monomer (10-Methacryloyloxydecyl dihydrogen phosphate) in its PANAVIA™ resin cement and CLEARFIL™ bonding systems creates a hybrid layer, which is critical to preventing recurrent decay. The hybrid layer is the interface between the tooth and the resin—and it is also what breaks down over time.
"The reason it breaks down is that it has gaps, which means the barrier is not complete. So, as the osmotic pressures of the tooth begin to flow and create pressure on that hybrid layer, you get a breakdown, and that's ultimately where the decay occurs," Dr Schmedding explains.
What makes MDP such a foundational chemical tool for preventing recurrent decay is how it facilitates an acid-based resistance zone, Dr Schmedding says. As the material polymerizes and cures, it creates calcium salt, an impermeable barrier essential to preventing recurrent decay and increasing the restoration's lifetime.
"Some of the materials have fluoride release, and those help fortify the hybrid layer over time, but that calcium salt and layering that acid-based resistance zone, or non-water-bearing membrane, so to speak, is what creates that longevity," Dr Schmedding says.
The Technique Component to Defend Against Recurrent Decay
However, no matter what adhesive system you use, Dr Schmedding thinks recurrent decay also results from the challenges of working in a very wet environment while incorporating a hydrophobicmaterial into it. Clinicians need to control that moist environment before placing restorative material with any success. Dr Schmedding says lack of isolation with a rubber dam, or Isolite or DryShield, makes things go awry regarding recurrent decay around restorations.
"You've got to control the environment to succeed," Dr Schmedding explains.
Dr Lawson agrees that a clinician's restorative technique with adhesive systems can prevent recurrent decay. He explains that a restoration that develops a strong bond with tooth structure without residual stress would be less likely to lead to a marginal opening. A marginal gap creates a space for bacteria to harbor.
"So good bonding protocol could help prevent secondary caries," Dr Lawson says.
In addition to excellent isolation, Dr Schmedding thinks clinicians need to remember the essential nature of adequate curing light. Most dentists do not take a deep dive into the curing light and its work. For most clinicians, seeing the material cured on the surface is proof that the light works. However, Dr Schmedding says that what happens below the surface is essential to prevent recurrent decay.
"You can cure the composite surface with your iPhone if you shine the light on it long enough. But what's happening down in that box form, the deepest part of the restoration? So, a reliable light source is critical along with isolation," Dr Schmedding explains.
Another technique-sensitive part of preventing recurrent decay is how clinicians handle the composite, meaning the thickness of the layers they place. Polymerization shrinkage is a constant, Dr Schmedding says, and clinicians' placement techniques will help mitigate those adverse effects on the margins of restorations.
"They are going to shrink today; they are going to shrink tomorrow; they are going to shrink for the rest of our careers," Dr Schmedding says about polymerized materials. "I like to use a small layer of flowable on the pulpal floor of the preparation in a minimal, .5mm layer to reinforce my hybrid layer. But I am placing at such a small increment that I'm not allowing polymerization shrinkage to pull away from the tooth structures."
The layering thickness is crucial. When dentists place too much composite and then cure it, the restorative material shrinks away from the bonding agent. Dr Schmedding says the shrinkage can also pull the bonding agent away from the tooth in some cases.
"Dentists are creating gaps and leakage right there just by overdoing it," Dr Schmedding says, adding the curing too fast or not curing enough doesn't help either. "If you have uncured materials down in the box, you don't get the physical properties or create a barrier against bacteria or leakage."
In addition to understanding composite placement techniques and the principles of polymerization, Dr Schmedding also uses Kuraray's KATANA™ Cleaner before placing his bonding agent or etchant. The cleaning agent removes any remaining fluids or biofilm down in the box form that could prevent a good bond.
"You don't want anything in-between there," Dr Schmedding says of the interface between the tooth and the bonding agent.
Dr Schmedding thinks that clinicians need to slow down regarding placement techniques generally. Today's restorative dentistry isn't like amalgam, which involves little to no finesse.
"It was pretty simple," Dr Schmedding says of the amalgam restorative technique. "You put a band around it and pack away. Today, it's all technique, or you will have problems."
Reference
J Antonucci, J., Dickens, S, D - Acrylics, Biomaterials Science (Third Edition), Academic Press,2013,Pages 103-111, ISBN 9780123746269,https://doi.org/10.1016/B978-0-08-087780-8.00012-7.(https://www.sciencedirect.com/science/article/pii/B9780080877808000127)
Greany, DDS T. Recurrent Caries - ToothIQ. ToothIQ.com. Published 2018. Accessed June 2, 2022 https://www.toothiq.com/dental-diagnosis/recurrent-caries/.
University of Toronto Faculty of Applied Science & Engineering. (2018, January 30). The fight against tooth decay gets help with a new smart material: Team designs new antimicrobial materials to prevent recurrent cavities under fillings. ScienceDaily. Retrieved June 1, 2022, from www.sciencedaily.com/releases/2018/01/180130123800.htm
Schnaider L, Ghosh M, Bychenko D, Grigoriants I, Ya'ari S, Shalev T, Shlomo Matalon A, Sarig R, Brosh T, Pilo R, Gazit E, and Adler-Abramovich, L Enhanced Nanoassembly-Incorporated Antibacterial Composite Materials, ACS Applied Materials & Interfaces 2019 11 (24), 21334-21342, DOI: 10.1021/acsami.9b02839, https://pubs.acs.org/doi/10.1021/acsami.9b02839