Care From Afar
Technologies help dentists connect with hard-to-reach patients and add convenience to treatment.
Care From Afar | Image Credit: DC Studio - stock.adobe.com

Access to care has long been a challenge for dentists and patients alike. While preventive care could prevent numerous oral health issues, it’s not accessible for a large percentage of patients—a percentage that has increased year over year.
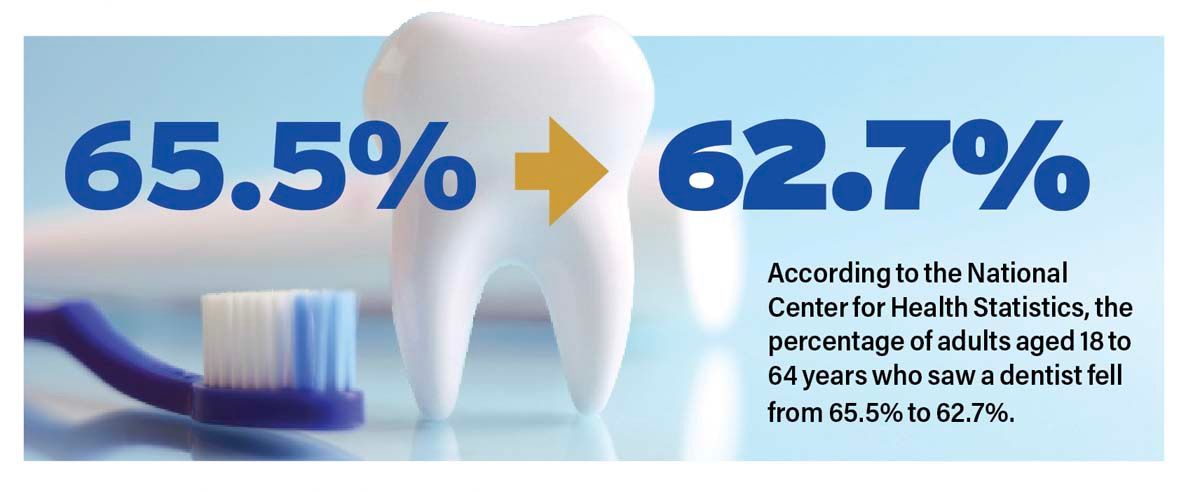
According to the National Center for Health Statistics, the percentage of adults aged 18 to 64 years who saw a dentist fell from 65.5% to 62.7% between 2019 and 2020.1 Some of the decline may be attributed to the onset of the COVID-19 pandemic, but the numbers are still moving in the wrong direction.
“There are plenty of challenges in treating hard-to-reach patients: Funding, the number of caregivers willing to do the work, proper financial incentive to provide the care, and the amount of equipment required to perform dentistry are the main challenges I see,” says Stuart Kazen, director of domestic sales for Aseptico Inc. “On the positive side, there is more recognition about the lack of access to care and more effort to fund dental care. There is better equipment and technology.”
This technology may be key to bridging the gap. By utilizing technology-supported remote services and mobile technology, dentists can better connect with hard-to-reach patients and add the convenience to treatment that will keep patients coming back.
“Emerging technology holds tremendous promise in overcoming oral health challenges, reducing disparities, and enhancing access to care through various avenues,” says Maria Kunstadter, DDS, CEO of The TeleDentists.
These avenues encompass many areas, including precision dentistry using cutting-edge technologies that enable personalized treatment plans designed to improve outcomes for diverse patient populations; telehealth and remote monitoring that can bridge the gap between underserved communities and dental care providers; digital health records and analytics; mobile applications that encourage self-monitoring; and artificial intelligence (AI), computer vision, and machine learning.
“Technology has brought about transformative changes in how dental health professionals interact with and reach underserved populations, including improved care coordination,” says Tina Saw, DDS, founder and CEO of Oral Genome. “In the past, underserved communities faced challenges due to limited access to dental care and outdated communication methods like paper charts and phone calls. However, with the advancement of technology, dental practices have been able to bridge the gap and better serve these populations through enhanced care coordination.”
Challenges to Care
Bridging the gap to serve these populations isn’t easy. In 2022, there were 7192 dental care health professional shortage areas (HPSAs) in the United States—meaning the 69 million people living in those areas had limited or no access to dental care. To remove the HPSA designations across the United States, 11,896 practitioners would need to join the workforce.2
This shortage of dental professionals and lack of access to care are particularly prevalent in rural communities, where 43% of people don’t have access to care.3 A 2019 study confirmed that people in rural areas were less likely to have seen a dentist in the prior year than patients in urban settings; 57.6% vs 66.7%, respectively.4
“One significant hurdle is the lack of access to dental care in these communities, often due to limited facilities and a shortage of skilled dental professionals who are willing to work in such areas,” Dr Saw says. “Geographical barriers further compound the problem, making it difficult for patients in remote or medically underserved regions to access dental services.”
Even within urban populations, many people face challenges in accessing care. Language barriers, limited health literacy, and disabilities create unique obstacles to providing necessary oral healthcare. Disparities are also closely tied to other social determinants of health, which affect several racial groups disproportionately. Between 2019 and 2020, 66.6% of White adults aged 18 to 64 years reported going to the dentist compared with 56.8% of Black adults and 55.3% of Hispanic adults.4
Financial differences also play into these disparities. Only 50.4% of adults in urban areas in homes with family income less than 139% of the poverty level received oral health care in the prior 12 months, while 79.3% of adults with income over 400% over the poverty level saw a dentist.4
“Financial constraints and inadequate dental insurance coverage prevent many individuals from seeking regular preventive care or timely treatment, leading to the exacerbation of dental issues,” Dr Saw says. “Overcoming these obstacles requires targeted efforts to improve access, increase provider availability, implement outreach programs, and develop culturally sensitive approaches to ensure that all individuals, regardless of their circumstances, have access to quality dental care.”
In addition to income barriers, insurance deficits also negatively impact access to care. One study found that only half the children enrolled in Medicaid saw a dentist in 2019.5 Medicaid is not required to provide dental benefits for adults.6
“The biggest challenge is our profession,” Dr Kunstadter says. “Who is reaching out to those populations? When you look at the number of medical doctors who accept Medicaid, it’s in the high 80%. Dentists in my state who accept Medicaid is 29%. We need to engage our profession to provide services to those who need our help.”
Teledentistry
Traveling to the dentist or even making room in a work schedule to go across town for an appointment can deter people from seeking treatment. To combat this, dentists are finding a way to bring treatment to people, instead of the other way around. Teledentistry is one way this is being accomplished.
“Why take half a day off from work or school to go into an office when the virtual consultation can be the solution?” Dr Kunstadter says. “For offices, why drag people in, use PPE [personal protective equipment], staff time, and chair time when a virtual consultation can solve the problem. It’s a learning curve for all new technology, but when implemented, will add innovation and improve workflow.”
With teledentistry, all it takes is an internet connection to have access to a dental specialist. Dentists can triage a problem, educate patients on home care, prescribe any necessary medications, and make assessments about whether the patient needs to come into the brick-and-mortar facility for hands-on care—all without the patient ever setting foot in the office.
“Virtual care helps patients be connected to that initial component of understanding the need for treatment and really eliminating the frustrations that are going to come up if you’re traveling an hour and a half to go see a doctor,” says Brant Herman, CEO and founder of MouthWatch and Dentistry.One. “If you have inflammation and need an antibiotic before your appointment, let’s get that done virtually. If you need to come in for treatment, let’s get the right stakeholders or family members on the call. If you have a follow-up appointment done virtually instead of in office, you’re more likely to attend it.”
In summary, Herman says, teledentistry gives clinicians the opportunity to educate the patient on why they should come in. They can address issues that might prevent a patient from going through with treatment before the appointment, allowing for a productive office visit when the patient does come in. The practitioner gets the opportunity to educate, reassure, and communicate all the things that might prevent treatment from happening, saving time and money for both the patient and the practice.
Care From Afar | Image Credit: Fotomomento01 - stock.adobe.com
“Virtual care is a game changer in providing care to more patients,” Dr Kunstadter says. “All offices should offer teledental services. It not only increases chair time by eliminating unnecessary trips to the dentist but also can reach new patients who want the convenience of teledental visits.”
Platforms such as TeleDent from MouthWatch are designed to improve patient outcomes with remote monitoring while improving chair time efficiency. Clinicians can message patients or have live video chats to discuss issues or treatments. TeleDent allows practitioners to store notes, visual treatment plans, tooth numbers, images, videos, and more in a patient record and share intraoral images with other specialists or providers.
For dentists who are hesitant to add teledentistry to their offerings, there are other solutions. Dentistry.One is a network of providers across the country. Working with an insurance company or rural health authorities, Dentistry.One connects patients with a dentist to do an evaluation, talk to the patient to get an understanding of their needs, and make initial treatment decisions such as calling in a prescription. If necessary, Dentistry.One can coordinate in-office care for the patient.
“Dentistry.One can then find a dentist who accepts their insurance that has an open time slot,” Herman explains. “We send an oral health report based on the virtual consult to the doctor, and they, without doing anything, have a new referral. They have a new patient coming in and they understand the need for treatment for that patient. We felt we needed to start bringing actual care delivery into the model.”
The TeleDentists is another digital teledentistry platform that provides teledentistry services to patients 24 hours a day. Patients can go online and get a virtual consult from a board-licensed dentist at any time, reducing the need for an emergency room visit. When follow-up visits are needed, appointments can be booked for the next day.
Teledentistry isn’t just a convenient tool to reach underserved populations; for many who go to the dentist regularly, it’s becoming an expectation. With the medical industry increasing digital offerings, patients are beginning to expect and want the same level of remote care from their dentists.
“The health care consumer is way more tech savvy and way more expectant of having visits virtually, when possible,” Herman says.
Remote Monitoring
Technology can also help identify potential health issues before they start. Through early detection, potentially severe problems can be avoided before they become critical. Remote monitoring applications make early detection and preventive care more accessible to hard-to-reach populations.
One such remote monitoring service is Oral Genome, whose saliva testing uses machine learning and computer vision to identify often-undetected oral health conditions. The patient takes the saliva test and scans it with their phone to get a wellness report that details their results and any high-risk factors. Patients can then consult with their dentist about any concerning areas.
“Oral Genome’s point-of-care dental saliva test allows for remote screening and early detection of oral health issues,” Dr Saw says. “Patients in dental deserts can use this screening tool to assess their oral health status and receive personalized prevention plans without the need to physically visit a dental office.”
Saw says technologies like Oral Genome, in conjunction with Harmony Health Foundation, offer promising opportunities for increased access to care in areas known as dental deserts.
“Harmony Health Foundation’s collaborative approach can integrate telehealth solutions, enabling virtual consultations between patients in dental deserts and dental professionals from other locations,” she says. “This real-time communication empowers patients to discuss their oral health concerns, receive advice, and access specialized care without the barriers of distance.”
And advances in technology are the foundation that is making this possible.
“The integration of AI, computer vision, and machine learning greatly facilitates early diagnosis and risk assessment of oral health conditions,” Dr Saw says. “By analyzing patient data and identifying patterns, these intelligent tools support dental professionals in making more accurate and timely diagnoses, especially in areas where access to specialized care is limited.”
Portable Dentistry
Technology is also supporting boots-on-the-ground efforts to bring care delivery to the patient. In March 2023, Congress passed the MOBILE Health Care Act, which expands the ability of community health centers to establish mobile clinics in underserved areas. Since 2019, there has been 40% growth in health center mobile units that bring care and treatment to patients outside the traditional office.7
“Oral disease is the most prevalent disease in the world and is almost 100% preventable,” Dr Kunstadter says. “With teledentistry, a dentist and a hygienist can educate auxiliary staff at schools, medical offices, and community health centers to provide the hands-on care to apply fluoride varnish, silver diamine fluoride, and more. Teledentistry is the tool to improve oral health and health equity for millions.”
Through teledentistry the midlevel provider can bring a dentist into the appointment virtually, and they can work as a dental team for more complex dental treatments. This is happening, for example, in remote areas of Alaska, where there are few dentists. In these settings, travel logistics and distances can be arduous. With technology, the dentist can be in more locations virtually while hygienists and dental therapists (depending on state-by-state regulations) can travel to the patients to provide care.
“A virtual dentist can be anywhere there is internet,” Dr Kunstadter says. “Access to the right specialist from a community health center can be key to improving oral health for that community.”
Providing care to remote areas is important but the benefits of mobile health clinics are far-reaching and can help other populations as well. Schoolchildren, geriatric or homebound patients or those with special needs, patients who are incarcerated, and underserved urban communities are all target populations for mobile dentistry.
To reach some of these populations, The TeleDentists is working with the National Minority Health Association (NMHA) to increase access to care. The NMHA’s goal is to help close the disparity gap in minor health and health care. The organization’s Operation Healthy You program identifies areas of health care disparities and works with health care providers—such as The TeleDentists—to address those needs.
“We are working together to improve health equity by increasing access to teledentistry and offering a training course for application of silver diamine fluoride when recommended by a virtual dentist,” Dr Kunstadter says. “This is a game changer for children as it could prevent small cavities from being emergency room visits in a few years and reduce the burden of poor oral health.”
In addition to teledentistry capabilities, advances in mobile technology allow for greater onsite treatment that might not have been possible in the past.
“Portable dentistry equipment continues to advance to be even lighter, better, and more capable than in years past,” Kazen says. “One of the biggest breakthroughs is the use of vacuum blower technology vs traditional air compression. In the past, portable dental delivery systems all used air compression to run the vacuum and handpieces. Today, new vacuum blower technology is preferred because it is just as powerful, quieter, and significantly lighter than traditional air systems.”
Other advances, such as the ability to run portable dental systems using battery power, have made dentistry even more mobile. With advancements in electric motors and batteries, some portable dental systems can operate for hours using battery power. This is incredibly convenient in rural areas with little access to power or in cases where the power has been knocked out.
One such system is the Aseptico GO Ultra Portable dental system, designed for performing restorative dentistry and dental hygiene. Compact and lightweight, the GO Ultra Portable can qualify as carry-on luggage. It can operate anywhere in the world; if there is no electrical power, there is an option for it to operate via a 24-V external battery.
“Aseptico helps dentists reach patients by designing and building portable dentistry solutions that dental professionals can rely on,” Kazen says. “The equipment has to do the job well; it has to be extremely reliable. Dentistry is demanding from an equipment standpoint and we don’t want the doctor to have to worry about whether or not their equipment is up to the challenge.”
The Future of Technology
Embracing technology in dental practices is perhaps one of the best opportunities to provide improved patient engagement, promote better understanding and management of oral health, and deliver quicker access to care for patients.
“Embracing technology is vital for increasing access to care at scale,” Dr Saw says. “Telehealth, mobile health apps, AI diagnostics, and remote monitoring enhance patient engagement and enable remote consultations. Seamless data sharing and interoperability that support comprehensive care coordination are essential in continuous health monitoring. Leveraging these technological advancements empowers patients, improves treatment outcomes, and fosters a more inclusive and accessible health care system.”
With technological advances emerging every day, opportunities for increasing access to care continue to expand. Technology like teledentistry and mobile dentistry is opening doors to close care gaps across the country—and the implications could be monumental.
“Incorporating these emerging technologies into oral health care practices with a focus on inclusivity and affordability can pave the way for a brighter future, where oral health disparities are minimized and quality care is accessible to all individuals, regardless of their circumstances,” Dr Saw says.
There’s still work to do, but the progress toward reaching all dental patients is encouraging.
References
1. Cha AE, Cohen RA. Dental care utilization among adults aged 18−64: United States, 2019 and 2020. Centers for Disease Control and Prevention. April 20, 2022. doi:10.15620/cdc:115597
2. Dental care health professional shortage areas (HSPSAs). Kaiser Family Foundation. September 30, 2022. Accessed August 23, 2023. https://www.kff.org/other/state-indicator/dental-care-health-professional-shortage-areas-hpsas
3. Rural America’s Oral Health Care Needs. National Rural Healthcare Association. Accessed August 23, 2023. https://www.ruralhealth.us/getattachment/Advocate/Policy-Documents/RuralAmericasOralHealthCareNeeds-(1).pdf
4. Cha AE, Cohen RA. Urban-rural differences in dental care use among adults aged 18−64. NCHS Data Brief, no 412. Hyattsville, MD: National Center for Health Statistics. 2021. DOI: https://dx.doi.org/10.15620/cdc:106856external icon.
5. Corr A, Wenderoff J. Inequitable access to oral health care continues to harm children of color. The Pew Charitable Trusts. March 11, 2022. Accessed August 26, 2023. https://www.pewtrusts.org/en/research-and-analysis/articles/2022/03/11/inequitable-access-to-oral-health-care-continues-to-harm-children-of-color.
6. Medicaid adult dental benefits: An Overview. Center for Health Care Strategies, Inc. September 2019. Accessed August 26, 2023. https://www.chcs.org/media/Adult-Oral-Health-Fact-Sheet_091519.pdf.
7. The Mobile Health Care Act: Everything You Need To Know. NACHC. June 14, 2023. Accessed August 23, 2023. https://www.nachc.org/resource/the-mobile-health-care-act-everything-you-need-to-know/.
