Can PPE Be Improved?
As with many infection control measures over the years, the need for personal air filtration manufacturing has arrived.
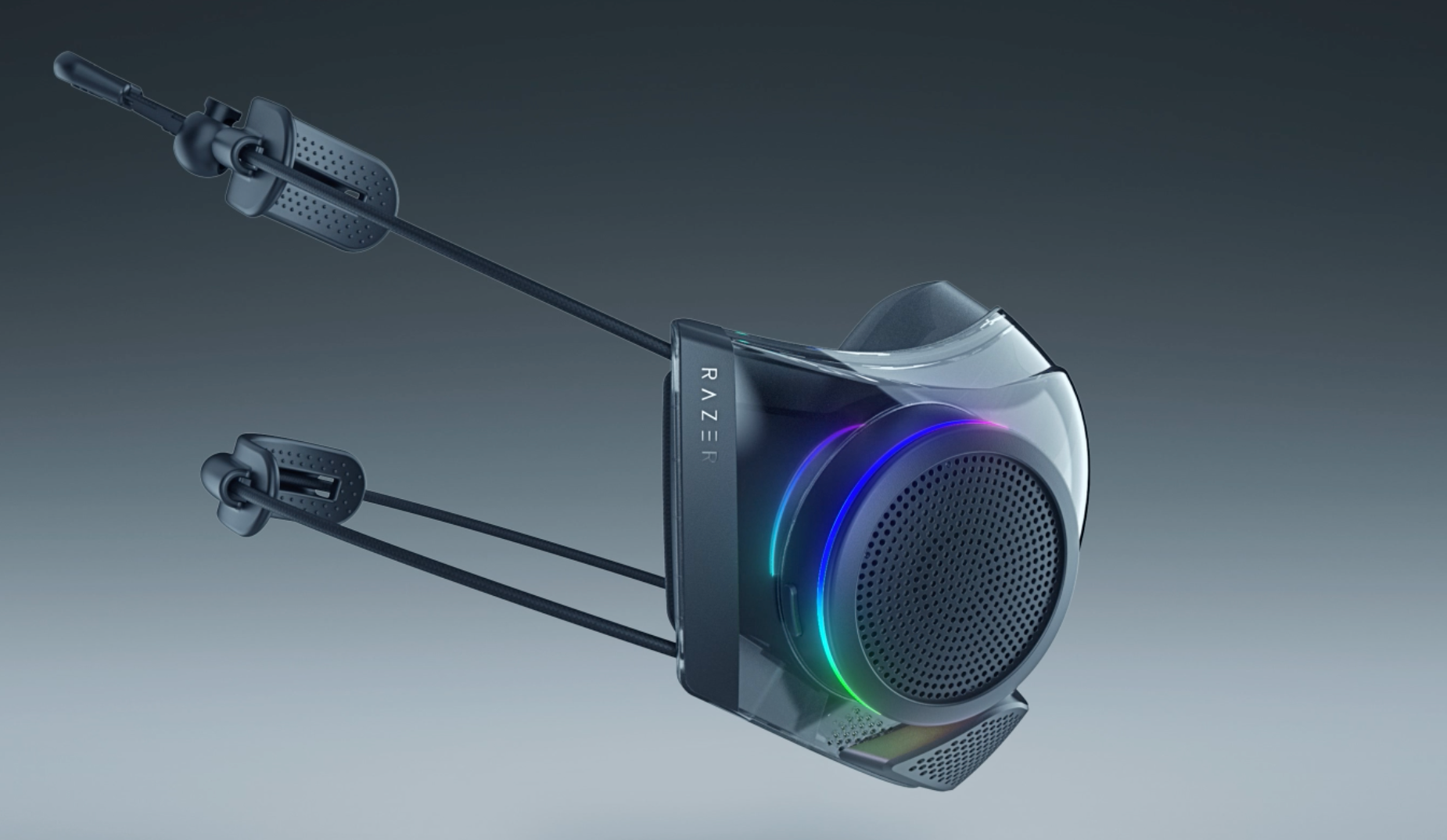
RAZOR ZEPHYR PRO
Technology can be an interesting critter sometimes. I say that because sometimes it can follow slow and predictable patterns while at other times it can take off in unexpected directions. Take Moore’s Law, for example, named after Gordon Moore, the co-founder of Fairchild Semiconductor and Intel Corporation. In 1965 Moore predicted that the number of components on an integrated circuit would double every 18 to 24 months. He was only using his gut and not some complicated mathematical formula, but that statement has held true for so long it is now known as a “law.”
Evolution
So what does Moore’s Law have to do with dentistry? Probably more than you might think, but my topic for this month focuses more on the evolution of our profession than anything else.
In my first 2 years of dental school, we did not wear gloves. I know that seems horribly antiquated and a tad nauseating to many of you, and that’s probably because both of those terms apply. But, we didn’t know any better.
Near the midpoint of my second year, there was a mandatory lecture for each class that spelled out the school’s new infection control protocol and procedures. At the time there were some concerns about losing tactile sensation due to wearing gloves and some other potential problems. I’m pretty sure the disease that drove the change didn’t even have a name at that point in time, but the profession stepped up and did the right things to ensure everyone’s safety. HIV is a tragic part of history, but it did drive dental infection control to where it needed to be.
Autoclaves were suddenly needed in every office, and we began running everything through them. Before the mid-1980s, dentistry did not steam sterilize handpieces and they were not designed to go through the abuse. Turbines failed almost as fast as they could be repaired. However, handpiece manufacturers rapidly designed and implemented changes to air turbines that allowed them to withstand the rigors of the autoclave.
And autoclaves themselves were flying out of warehouses as offices rushed to meet the new infection control protocols. When I graduated and began looking for my professional home, one of the first questions I had was, “Do you have an autoclave?” Sometimes the answer was “no,” and I would politely move on to another office.
Changes
I have been in the trenches since pre–“bloodborne pathogens standards,” and I have seen a lot of changes and improvements in our infection control devices.
I’ve seen latex gloves go powder-free and then latex gloves be overtaken by nitrile ones, which, at least for me, provide a much better tactile response and no allergies. I’ve seen handpieces go to ceramic bearings that withstand high-pressure steam and high temperatures, barriers that can inhibit cross-contamination, and custom-created optics that allow us to perform procedures under high magnification.
In the over 30 years since dentistry embraced wearing gloves and masks to help protect everyone from the transmission of diseases, our profession has seen incredible advances and changes in myriad products.
Yet it wasn’t until the sudden and unexpected arrival of SARS-CoV-2 and the resultant COVID-19 that dentistry turned to the concept of protecting our patients, our teams, and ourselves by utilizing snug, form-fitting, high-filtration respirators.
Up to that point, the prevailing wisdom appeared to be “any mask will do.” We paid little heed to the gaps at the sides of our masks or the fact that many particles were capable of passing straight through the limited filtration material they were composed of. The concepts of a Level 1, 2, or 3, or an N-95, were foreign to most of us, and we proceeded in blissful ignorance until the tidal wave of a novel coronavirus washed over us.
Moving Forward
In our current environment, perfect fit is important, especially when it comes to masking. Not only does a mask need to provide adequate filtration, but it also needs to fit in a manner that all inspired air passes through the filtration medium and not through gaps due to poor fit. Yet comfort needs to be factored in as well. Most of us understand all too well the trauma inflicted on our ears by masks whose ear loops pull tight to ensure a proper seal along the borders.
I challenge the manufacturing sector of our profession to come up with something that can solve this problem. The dental industry is uniquely prepared to help overcome these limitations.
What I envision is a high-quality reusable facial respirator that is custom-fitted to the face of the user. We can scan teeth with incredibly high accuracy—enough to meet the tough standards of the profession—so let’s scan a face in the same manner. If we can scan a tooth with 50-µm accuracy, imagine what a respirator milled or printed to match your facial contours would be like. We would have a perfect fit that would not permit any kind of leakage around its perimeter.
The frame could then use a high-filtration medium in detachable filters that could be removed and replaced as often as the user required. While we’re brainstorming, let’s add in some antiviral LEDs. Studies show that light emitted at the 264-nm range is very effective at killing germs, bacteria, and most importantly, viruses. Whatever pathogens (if any) managed to squeeze through the filters would be immediately exposed to the energy emitted by the LEDs, which would add another degree of safety.
Many of us working in N-95s every day battle the problem of our glasses fogging. The custom-fit would probably decrease that, but to help with that and for comfort, a couple of small cooling fans could be added to help more air inside the device. The exhaust fans from the device would also pass air through filtration to protect the user from potentially passing anything back out into the room air.
If the seal and filtration are well created, it might make our voices harder to hear. Perhaps a small speaker could amplify the voice under the respirator. That would be pretty simple to add-in.
The LEDs, speaker, and built-in cooling fans could be powered by a lithium-polymer battery that would last all day on a single charge. We would recharge the respirator every night just like we recharge our LED headlights.
These are the features that came to me as I was daydreaming about this project, and I’m sure this isn’t pie in the sky. I’ve seen some masks that sort of follow this idea that are already available, although none have been sold as “medical grade.” For a peek at one such device, take a look at the RAZER ZEPHYR PRO (razer.com).
Wrapping Up
This may seem like overkill but think back to 2020 when we all thought a Level 2 surgical mask was just fine. Since returning to my office in the late spring of 2020, I have continued to work in an N-95 mask because I simply feel it is safer for me and my patients.
Is a custom respirator like this going to be expensive? Well, there is no doubt it would be more expensive than current solutions, but we spend lots of money on things such as magnification and other items. I think the comfort and safety of something like this would be well worth the initial expenditure.
We’ve upgraded and improved many of our other infection control systems. It’s now time for dental manufacturers to improve the comfort, safety, and ease of use of personal air filtration. This is definitely an idea whose time has come. If you are thinking of developing such a product, contact me right now. I’ve got even more ideas.

ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.