Tackling a common issue with restoring implants
How a new solution achieves the advantages of provisionalization with the convenience and efficiency of conventional healing caps.

How did you decide to team up and tackle emergence profile issues?
MB: I’ve been referring my surgical cases to Todd since he came out of residency. In 2012, we had a particular patient who I had referred for an implant on an upper cuspid. The implant was placed well, and the site had healed nicely. However, placing the crown was a very frustrating experience. I had to spend about an hour and a half cutting away nice healthy tissue to make it fit.
Of course, the lab tech was forced to reconcile the emergence profile of a natural-looking crown with the site left by a conventional round healing cap. Cuspids aren’t round, so there’s no way a round healing cap creates an emergence profile that works well for a regular cuspid. I shared the story with Todd and that got us thinking about a better way to do this.
Trending article: How to avoid restorative Class II blues
Is this a common scenario in restoring implants?
TL: Yes, very much so. First let’s be clear-you need good impressions and an experienced lab technician. But, even when that’s true, we still see these situations.

In the case Mark referenced, the lab tech did the right thing by providing an anatomic emergence profile. But, it didn’t fit the tissue shape created by standard round healing caps. So, labs typically under contour restorations-they don’t make them as anatomic as they can be-because they know the result may be lots of soft tissue manipulation during the restorative appointment for the dentist and pain for the patient. That happens enough and the dentist switches labs.
There’s been a disconnect with the whole team as far as soft tissue management. We’re cutting tissue away at restoration time because the emergence profile of the crown is wrong. The crown is wrong almost by design because we don’t provide the lab with the correct soft tissue emergence profile to begin with. It’s a backward way of doing things.
What are the patient implications of not managing an emergence profile?
TL: Patients expect form and function, although they don’t use those terms. When they invest thousands of dollars, they expect implants to look as natural as, or better than, their original teeth. They’re disappointed if they see black triangles or have molar pockets causing food impaction. And as their dentists, we’re just as disappointed when we see those problems.
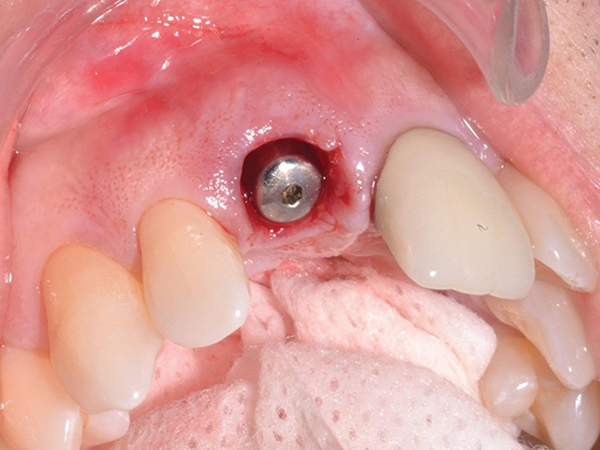
A traditional round healing cuff and the resultant emergence profile. Non-anatomical shape and poor tissue condition set the stage for poor implant esthetics and function.
When Mark approached me in 2012, I thought to myself, “I do a lot of implants, but it’s not always fun.” I get patients who come back from the restorative dentist saying, “I just spent $4,000 and look at this.” We could be batting .900 in what I call “Aesthetic Average.” At present, I’m not sure dentistry is batting over .400 when it comes to implant esthetics and related function. Proactive soft tissue management can close that gap.
Continue reading on page two...
What is state-of-the-art in emergence profile management today?
MB: We’ve talked about the shortcomings of traditional round healing caps. They’ve been around since the early days of implant dentistry.

Establishing emergence profile with the Gingival Cuff Links healing cuff. The T-Handle provides a gripping surface and acts as a visual guide to confirm proper implant orientation.
Provisionalization, where interim abutments are built out with esthetic materials, has also been around for some time. Clinically speaking, it’s a good solution for soft tissue management. In the last few years, provisionalization has enjoyed a bit of a resurgence as a hot topic on the lecture circuit. Unfortunately, it’s tedious and time-consuming, so few dentists take this route.
In the last several years, attempts to modernize and improve traditional healing caps have been introduced. One contoured healing cap system made from PEEK (Polyetheretherketone) offers a range of shapes and sizes for an incrementally more anatomical fit. Unfortunately, PEEK is hard to cut, so they can’t be adjusted; they either fit or they don’t. There’s also a system made of PMMA (Polymethyl methacrylate) that we tried in our research but found to break under loading.
Read more: Changing the implant workflow
Todd and I have spent the last seven years developing our solution called Gingival Cuff Links, which will launch later this year at the AAOMS and AAID.
Would you tell us a little about the Gingival Cuff Links technology?
MB: Our goal with Gingival Cuff Links (GCL) has been to achieve the advantages of provisionalization with the convenience, ease of use and chairside efficiency of conventional healing caps. We set “must-have” design objectives of adaptability, durability and reliability. Finally, we wanted a solution that would be practical for widespread use by our colleagues across specialties, so low cost and office visit efficiency have been priorities.

Gingival Cuff Links emergence profile. The ability to consistently create an anatomical emergence profile allows for implant restorations that fit well and look natural.
As a maxillofacial surgeon/restorative dentist research team, you can imagine development has consisted of years of chairside trials and refinement. As mentioned earlier, we tried a range of materials until we arrived at the current sculptable bis-acryl body cuff fused to specially modified interim abutments that are titanium-based. The patented T-handle feature, which maintains proper orientation relative to the implant, came from on-the-fly modifications that Todd made because initial molds made from stone were difficult to hold, drill and adjust.
Todd and I set the bar at 500 successful cases before we would even show a design to colleagues. Now, six years later, we have thousands of successful cases. And we’ve seen our own Aesthetic Average climb to well over .900.

ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.