Educating Dental Patients about Mask Myths
© Robert Petrovic/Adobe Stock

Last weekend was one of those times when I felt so uncomfortable, I wanted to shout a public health message from the rooftops. Instead, I mingled with the locals in silence, but later on, I submitted a yelp review that contained a pointed but gentle message. Let me explain.
On a busy Friday, I entered a local lunch establishment in Warm Springs, Georgia, and stood in line for a take-out order. I live in the deep south where the economies of small towns like Warm Springs aren’t too different from the early 1900s, when Franklin Delano Roosevelt first arrived, hoping to find a cure for polio.1 Swimming in the 88 °F spring waters didn’t bring him the cure he was looking for, but he developed New Deal Programs based on his observations of poverty and poor living conditions. As is the custom in some restaurants in the area, I could hear traditional Christian music playing softly in the background. As I stood in line, I noticed that I was one of only two patrons donning a mask. To my surprise, none of the staff were wearing masks either, and a couple of the women who were serving customers looked like senior citizens.
My frustration is with Georgia locals who refuse to wear masks indoors for political reasons or because they perceive that some of the public health guidance, such as mask-wearing, are direct threats to their freedoms. I’ve even noticed locals who mock those who wear masks, and then others like me want to shame or report those who don’t. Wearing a mask has become controversial, and it has been politicized in part because political beliefs affect how people process scientific information.2
The science on the wearing of medical/surgical masks and alternative mask materials in the public domain has evolved rapidly and engineering professors are feverishly running tests, especially in light of coronavirus disease 2019 (COVID-19) mask shortages.3 While following aerosol researchers and their daily tweets and research publications, I’ve learned a lot more about the science surrounding mask efficacy during the COVID-19 pandemic.
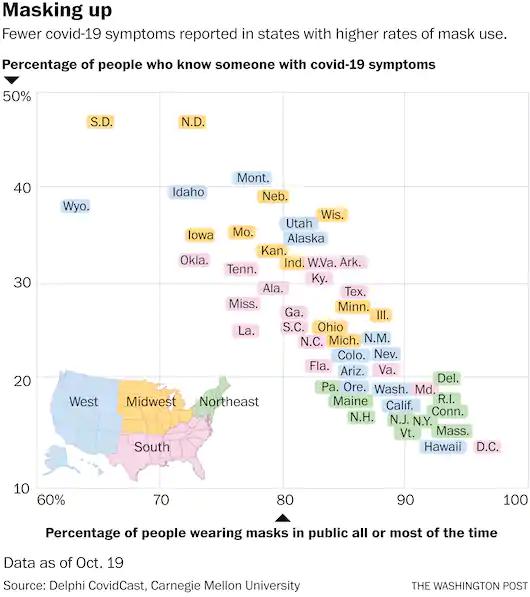
Washington Post—October 23, 2020
Environmental engineering professor Linsey Marr from Virginia Tech University is an expert in the airborne transmission of infectious disease, and she and her colleagues are testing the efficacy of various masks in filtering out different particles.3 Due to sluggish personal protective equipment (PPE) supply chains, the medical/dental community, and the public improvised with alternate materials.3 Other possible reasons for mask material alternatives include lack of education, disability, cost, the discomfort of N95 respirators, and other health-related issues, such as respiratory problems and low tolerance of masks covering the mouth and nose. Marr’s research team also works to problem solve by sourcing off-the-shelf, affordable materials for homemade masks that meet scientific criteria in filtering SARS-CoV-2 particles.3 One of the homemade mask materials that filtered out at least 80% of particles was microfiber cloth (used to clean eyeglasses). There were also material failures, such as heavyweight cotton t-shirts, shop towels, and shop rags that, when tested, only filtered out 10% of the smallest particles and about 50% of larger particles. Experiments are ongoing, and the team shares results on Twitter in real-time. Other aerosol science labs around the United States adopted Marr’s methods and are testing materials in different regions as well.2
Aerosol Transmission of SARS-CoV-2
We now know a lot about how SARS-CoV-2 travels around in the air. When SARS-CoV-2 first started to spread, health officials were initially worried about the transmission of droplets, which are larger particles that are heavier and travel less than 6 feet. The social distancing rule of staying 6 feet away from people made sense until aerosol researchers discovered that small aerosol particles could remain in the air for hours and transmit the virus.4
Researchers initially thought that SARS-CoV-2 was transmitted through droplets and fomites, but there was growing evidence of airborne transmission.5,6 Researchers are still working hard to better understand specific settings that facilitate super-spreader events.
Second Wave: Time to Educate
I recently read a better analogy for the expected second round of SARS-CoV-2. Instead of calling it a second wave, Michael T. Osterholm, PhD, MPH, the director of the Center for Infectious Disease Research and Policy at the University of Minnesota, calls the coronavirus pandemic a forest fire.4 Just like California and Oregon, the massive raging fires have been suppressed in some spots but have not been put out completely. As long as the fires have fuel and the right environmental conditions, they will keep burning.
Case counts of COVID-19 are beginning to rise as colder weather is forcing more people indoors.7 As the numbers continue to grow and the constant bombardment of news media reports of gloom and doom continues to heighten anxiety, our patients may appreciate random acts of kindness and consideration in unexpected ways. In addition, many of our patients look up to us—dentists, dental hygienists, and dental assistants—as having expertise in oral and general health care disease prevention, particularly if we act professionally in our demeanor, appearance, and conversation. We have unique opportunities to educate and inform our patients about COVID-19 prevention, and we can give them unbiased, objective information based on science. By modeling PPE to minimize exposure and by following a complete hazard control program, our strategies send a positive message to patients.
So, what should I tell my patients about protecting themselves and the wearing of masks?
Marr recommends educating people to remember the 3 Cs and 1 M listed below:2
- Avoid Close contact situations. Maintain distance from other people. Six feet doesn’t mark a magic barrier, but the particles do dilute with space.
- Avoid Crowds. Being in large crowds increases the chances that one will be around someone infected with the virus and that the virus will spread to others.
- Avoid Closed, poorly ventilated spaces. Imagine sharing a room with a cigarette smoker. Will I take in any smoke while sharing this space?
- Wear Masks. According to Marr, research shows that layering fabric improves a mask’s effectiveness. A single layer of fabric helps some, but 2 layers should block 95% of particles.
Below are a few of the most frequently asked questions about masks for the general public, and we can share the answers with them as appropriate.
What is the best type of mask?
The effectiveness of a mask depends on 2 main factors: how well it fits and how well the chosen material filters out aerosols of different sizes. A properly fitted N95 respirator filters out at least 95% of aerosols of all sizes. Do not use N95 respirators with valves because they allow aerosols to escape and do not protect others.8 If you choose to wear an N95 respirator with a valve, cover the valve with a piece of tape. Surgical masks offer protection in the range of a 70% to 80% filtration rate, but there is wide variability depending on the brand. Cloth masks with filters are a good choice, while materials like vacuum bags, HEPA filters, and MERV 13 filters appear to work well. Homemade masks made out of tea cloth or cotton t-shirt material offer about 50% protection. Masks should be worn completely covering the mouth and nose when indoors with other people except in your own residence or vehicle.9
Should I wear a mask outside?
Wear a mask outside when you are around or are passing by others at a close distance like an urban sidewalk. It is good etiquette to ensure adequate space between you and another person or wear a mask during the encounter.9
How important is the proper fit?
Mask fit is of utmost importance to prevent aerosols from entering gaps. If your mask fits well, it will suck up against your nose and mouth when breathing in.9
Is it OK to remove my mask to talk?
It is not OK to remove your mask to talk unless you are outdoors and away from people. When speaking, about 10 times more respiratory aerosols are emitted, and when singing or yelling, respiratory aerosols emitted can be about 50 times more. Do not allow others to talk to you without a mask when they are within close distance.9
Are transparent masks safe?
Transparent masks may be safe if they seal around the face and nose (without gaps), but the material has to filter aerosols and should not fog.9
How can I assess my mask at home?
Inspect your mask, better yet, have someone else inspect it for visible gaps while talking or singing. If the mask fits well, the air passing through the mask will push closer to your face while inhaling and away from your face while exhaling. Researchers from Georgia Tech University suggest testing fabrics by their ability to block water droplets. Use a spray bottle and a mirror for this purpose.9
Are face masks and face shields interchangeable?
No. Face shields do not offer much protection against aerosols.9 They are used by health care professionals as a supplement to masks for partial eye protection but are should not be substituted for safety glasses as face shields are less useful.9
By modeling appropriate PPE, including face masks, we show patients who we are, and we can share what we’ve learned to save lives. Walk the talk, share your expertise, and do your part to mitigate the spread.
References
1. National Parks Service. Warm Springs Historic District, Georgia. Accessed Oct. 1, 2020. https://www.nps.gov/nr/travel/presidents/roosevelts_little_white_house.html
2. Irby S, Nelson E. Spurred by COVID-19, researcher Linsey Marr evaluates efficacy of sterilized N95 respirators, alternative mask materials. Virginia Tech Engineering. Accessed October 1, 2020. https://eng.vt.edu/media-center/articles/2020/spurred-by-covid-19-researcher-linsey-marr-evaluates-efficacy-of-sterilized-n95-respirators-alternative-mask-materials.html
3. Aerosols vs. droplets: in transmitting COVID-19, there’s a big difference. Yale School of Engineering & Applied Science. September 1, 2020. Accessed October 1, 2020. https://seas.yale.edu/news-events/news/aerosols-vs-droplets-transmitting-covid-19-there-s-big-difference
4. Reilly M. Osterholm: Forget waves, this pandemic is a 'forest fire'. Minneapolis/St. Paul Business Journal. June 22, 2020. Accessed October 1, 2020. https://www.bizjournals.com/twincities/news/2020/06/22/osterholm-interview-covid-19-forest-fire.html
5. Chau N, Hong N, Ngoc N, et al. Superspreading event of SARS-CoV-2 infection at a bar, Ho Chi Minh City, Vietnam. Emerg Infect Dis. 2020;27(1). doi:10.3201/eid2701.203480
6. @Lindseymarr. CDC's new guidance is out: "COVID-19 can sometimes be spread by airborne transmission" October 5, 2020. Accessed October 5, 2020. https://twitter.com/linseymarr/status/1313172475988062208
7. Wan, W, Dupree J. Coronavirus cases are rising in U.S., sparking worries the next big wave has begun. Washington Post. October 13, 2020. Accessed October 15, 2020. https://www.washingtonpost.com/health/2020/10/13/coronavirus-cases-rising/
8. Godoy, M. Yes, Wearing Masks Helps. Here’s Why. NPR. June 21, 2020. Accessed Oct. 15, 2020. https://www.npr.org/sections/health-shots/2020/06/21/880832213/yes-wearing-masks-helps-heres-why
9. Marr L, Miller S, Prather K. FAQs on Protecting Yourself from Aerosol Transmission. Accessed October 6, 2020. https://docs.google.com/document/d/1fB5pysccOHvxphpTmCG_TGdytavMmc1cUumn8m0pwzo/mobilebasic#h.64ykx5xjtlsy
Graph courtesy of the Washington Post—October 23, 2020