Study on parasite may improve the treatment of periodontitis
For the first time, researchers have shown that a unicellular parasite commonly found in the mouth plays a role in both severe tissue inflammation and tissue destruction. The study may improve the treatment of periodontitis.
For the first time, researchers from Charité – Universitätsmedizin Berlin have shown that a unique cellular parasite commonly found in the mouth plays a role in both severe tissue inflammation and tissue destruction. Most patients with severe and recurrent periodontitis (gum disease) showed an increased presence of the amoeba Entamoeba gingivalis inside their oral cavities.
The effect of this amoeba is similar to that of Entamoeba histolytica, the parasite responsible for causing amebiasis. Once the parasite has invaded the gingival tissue, it feeds on its cells and causes tissue destruction. According to the researchers' findings, which have been published in the Journal of Dental Research, the two amoebae show similar mechanisms of tissue invasion and elicit a similar immune response in the host.
Periodontitis is an inflammation of the gums and supporting structures of the teeth. It is one of the most common chronic diseases in the world. In Germany, approximately 15 percent of people are affected by a particularly severe form of this disease. If left untreated, periodontitis will lead to tooth loss. The disease also increases the risk of arthritis, cardiovascular disease and cancer. In patients with periodontitis, a decrease in the diversity of the oral flora coincides with an increase in the frequency of E. gingivalis. A team of researchers, led by Prof. Dr. Arne Schäfer, head of the Periodontology Research Unit at Charité's Institute of Dental and Craniofacial Sciences, was able to show that oral inflammation is associated with colonization by the oral parasite E. gingivalis.
Scientists have long been aware of the virulence potential of this genus of amoebae. The gastrointestinal parasite E. histolytica, for instance, causes a disease known as amebiasis, one of the most common causes of death from parasitic diseases worldwide. "We have shown that an amoeba like E. gingivalis, which colonizes the oral cavity, will invade the oral mucosa and destroy gingival tissue. This enables increased numbers of bacteria to invade the host tissue, which further exacerbates inflammation and tissue destruction," says Schäfer.
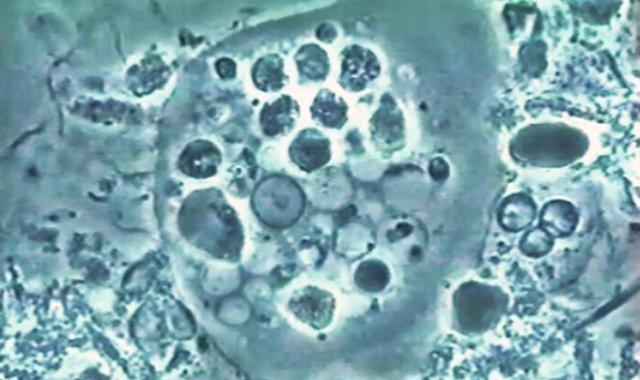
The international team of researchers was the first to describe precise roles of E. gingivalis in the pathogenesis of inflammation. During their analysis of inflamed periodontal pockets, the researchers detected evidence of the amoeba in approximately 80 percent of patients with periodontitis, but in only 15 percent of healthy subjects. Their observations revealed that, after invading the gums, the parasites move within the tissue, feeding on and killing host cells. Cell culture experiments showed that infection with E. gingivalis slows the rate at which cells grow, eventually leading to cell death.
The researchers concluded that the amoeba's role in inflammation shows distinct parallels to the pathogenesis of amebiasis. "E. gingivalis actively contributes to cell destruction inside the gingival tissue and stimulates the same host immune response mechanisms as E. histolytica during its invasion of the intestinal mucosa," explains Schäfer. "This parasite, which is transmitted by simple droplet infection, is one potential cause of severe oral inflammation."
Treatment success is often short-lived in patients with periodontitis. This might be due to the high virulence potential of this previously unnoticed, yet extremely common amoeba. Summing up the results of the research, Schäfer says: "We identified one infectious parasite whose elimination could improve treatment effectiveness and long-term outcomes in patients with gum disease." He adds: "Current treatment concepts for periodontitis fail to consider the possibility of infection by this parasite or its successful elimination." A clinical trial is underway to determine the extent to which the elimination of this amoeba might improve treatment outcomes in patients with periodontitis.
[ Editor’s Note: Materials provided by Charité – Universitätsmedizin Berlin. ]
References
1. X. Bao, R. Wiehe, H. Dommisch, A.S. Schaefer. Entamoeba gingivalis Causes Oral Inflammation and Tissue Destruction. Journal of Dental Research, 2020; 002203452090173 DOI: 10.1177/0022034520901738
2. Charité – Universitätsmedizin Berlin. "Improving the treatment of periodontitis." ScienceDaily. ScienceDaily, 15 April 2020. <www.sciencedaily.com/releases/2020/04/200415132825.htm>.