Sleep Apnea in Dentistry: The Business of Treating the Disorder
Dentists are well-positioned to help patients with obstructive sleep breathing, however, if they're thinking adding appliance-based therapy to their practices will create another profit center, they need to think again. Experts say effective sleep therapy happens when dentists commit themselves to being properly educated on the condition. It also requires collaboration with physicians, something that hasn't happened historically in dentistry.
Dentists are well-positioned to help patients with sleep apnea. However, they must prioritize educating themselves on the condition and working closely with physicians.
Late-night parties, exam-cramming, or Netflix marathons that extend into the wee hours of the morning may be why so many patients seem ready to doze off in the operatory — or not. Instead, it could very well be obstructive sleep apnea that’s to blame.
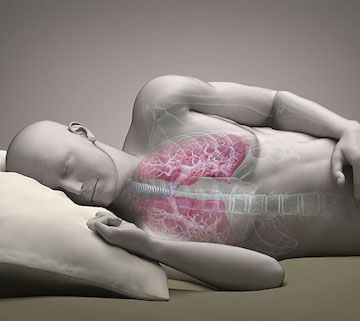
The Mayo Clinic defines obstructive sleep apnea (OSA) as “a potentially serious sleep disorder” that “causes breathing to repeatedly stop and start during sleep.” And it’s far from rare: According to the American Academy of Sleep Medicine (AASM), more than 25 million American adults have OSA. Harold Smith, D.D.S., president of the American Academy of Dental Sleep Medicine (AADSM), estimates that 20 percent of a dentist’s general practice is composed of patients with undiagnosed OSA.
RELATED: More Sleep Apnea Coverage
· New Organization Educations Dentists on Sleep Apnea
· What You Need to Know about Sleep Apnea
· Dentist Grows Practice Through Dental Sleep Medicine
“If a dentist is oriented to looking and screening for OSA, he’s going to be a very productive dentist in helping his patients have better qualities of life, catching serious comorbidities early, and possibly saving a life or two along the way,” Smith says.
GROWING AWARENESS
Smith recalls that in 1993, the field of dental sleep medicine was in its infancy. There were no studies or evidence-based literature for dentists to rely on. Education was anecdotal, based mostly on talking to practitioners who had begun treating patients. But over the last 25 years, Smith says, there has been “a virtual explosion” of literature, evidence-based studies, and clinical trials.
“We’ve come a very long way,” he says. “We’ve come to the point where oral appliance therapy is recognized as a viable option” for treating adult patients with OSA who are intolerant of continuous positive airway pressure (CPAP) therapy.
Oral appliance therapy features a custom-fit oral sleep appliance that fits into a patient’s mouth, much like a sports mouth guard or an orthodontic retainer. It supports the jaw in a forward position to help maintain an open upper airway.
Medical studies have helped physicians understand that oral appliance therapy is a modality of treatment they can consider for patients who are diagnosed with OSA. But what has lagged, says former AADSM president B. Gail Demko, D.M.D., with Sleep Apnea Dentists of New England in Weston, Massachusetts, is an adequate number of educated dentists to fill the need physicians are creating.
IMPORTANCE OF EDUCATION
Demko explains that OSA treatment is not an extension of what dentists learn in school. Crafting an appliance might be, but by engaging in oral appliance therapy, dentists are treating a medical disease, which falls outside of the typical dentist’s comfort zone.
“It’s incumbent upon us to understand that disease at the level of the physician, and dentists aren’t used to that,” Demko explains. “Any dentist can make one of these devices, but that isn’t the issue. The issue is understanding when to use them, when not to use them, and how the medical concerns of the patient play into it.”
Smith echoes those thoughts. OSA is not the usual type of profit center dentists bring into their general practice. Continuing education for many dentists, Smith explains, is going to a weekend course in periodontics, picking up a few pearls and bringing them back to their practice, and on Monday morning putting those pearls to use.
“Dental sleep medicine is an entirely different thing,” Smith says. “Dentists need to understand that obstructive sleep apnea and snoring are medical conditions, and we as dentists are treating these medical conditions. So the important thing for dentists to understand is they must be a valued part of the medical team in their community. And to become a valued part, you need to be properly educated.”
Story continues on the next page.

First, dental patients must receive a diagnosis from a physician.
PROACTIVE ROLE
Patients with OSA must first be diagnosed by a physician, and the patient can then be referred to a dentist. But dentists can play an important primary role in terms of screening. Smith points out that a dentist often sees a patient more frequently than does that patient’s primary care physician.
“Standard care for every patient who comes into a dental office for an examination is an oral cancer screening,” he says. “And an extension of that … is screening for obstructive sleep apnea.” During an oral cancer screening, a dentist can look for the anatomical markers that are fairly common in most OSA patients.
RELATED: More Practice Management Coverage
· Why You Should Market to Millennial Moms
· BIOLASE Launches New All-Tissue Laser System
· 4 Ways to Prevent IT Rip-Offs
He cautions, too, that it’s important not to pre-judge patients. “All of us have patients who you would never think have sleep apnea because they’re fit, thin, active and young,” Smith says. “But anatomically, their airway closes at night.”
Demko is also an advocate for screening, favoring a method called the STOP-Bang Sleep Apnea Questionnaire that’s used by physicians. It takes into account a range of criteria, including snoring, fatigue, blood pressure, and body mass index.
“There are no studies supporting that a physical examination of a crowded oral pharynx leads to sleep apnea,” Demko says. “But the STOP-Bang Questionnaire is highly indicative of obstructive sleep apnea, and it’s used by anesthesiologists screening patients prior to general anesthesia.”
COLLABORATIVE EFFORTS
In July 2015, the AASM and the AADSM issued the first joint clinical practice guidelines for oral appliance therapy. The guidelines are a pathway for sleep physicians and dentists to work together to treat OSA.
It’s not the only collaborative effort underway. In February, the AASM held Sleep Medicine Trends 2017 in Phoenix, Arizona, and dentists were invited to collaborate with physicians in a day-and-a-half workshop, “Oral Appliance Therapy: A Model for Physician-Dentist Collaboration.” Demko was one of the participants.
“It was huge,” she says of the first-of-its-kind collaborative workshop. “The more that physicians understand that we are there to give them another modality for treating their patients that may be more acceptable, more comfortable, and that improves compliance, the better.”
Demko notes that in Europe, about half of all patients with mild to moderate sleep apnea receive oral appliances as a first-line therapy. “It’s nowhere near that in this country because physicians give us two pushbacks,” she explains. First, physicians worry that dentists may not understand the fine points of adjusting devices, as well as the related medical aspects. Second, they’re afraid of losing patients to dental offices, and that patients won’t return for proper follow-up.
It’s up to the dentist to allay physicians’ fears, says Demko. “In the past dentists haven’t been playing as team members,” she admits. “And I think now with Trends, where the AASM is giving us a true chance to come in and be a part of the team on an equal standing with physicians, that’s going to make a huge difference in how physicians perceive oral appliance therapy.”
Story continues on the next page.

Profiting from sleep treatment requires a dentist to dedicate themselves to education.
ADA WEIGHS IN
The American Dental Association (ADA) is also taking an active role, having recently drafted a Proposed Policy Statement on the Role of Dentistry in the Treatment of Sleep-Related Breathing Disorders. Craig Ratner, D.M.D., of Staten Island, New York-based Exceptional Dentistry, and a national, state and local delegate of the ADA, says the association recognizes the need for a decisive policy to better define dentists’ role.
“Sleep apnea and sleep-related disorders are unique in that they are a medical condition that can be treated through some sort of dental intervention, or through the use of oral appliances,” Ratner says. “Dentists can definitely play a major role providing those services to mitigate the conditions.”
RELATED: More Practice Management Coverage
· Legal Advice for Proper HIPAA Compliance
· Dentist Puts Lid on Fraud and Embezzlement
· Why Dental Charts are Especially Appealing to Identify Thieves
Ratner agrees that dentists are well situated to recognize patients’ OSA symptoms and then collaborate with their medical colleagues. “And not only to collaborate with them, but to educate them on dentists’ and dentistry’s role in the treatment of this medical condition,” he says.
FINANCIAL CONSIDERATIONS
Smith believes that because so many people have OSA, providing treatment can be profitable for dentists who are willing to undertake the proper educational steps. “If a dentist can position himself—through proper education, through networking with his community physicians, through being proactive in screening and finding out about local sleep centers—he can create a network of physicians who respect the fact that he is prepared, he is educated,” Smith explains. “And physicians will refer patients to him. Then, if you create a significant number of people coming in for your services, it can be very financially rewarding.”
Demko, though, offers a caveat. She found that she was unable to work oral appliance therapy into her general practice because it’s essentially different from the way a restorative dentist works. A restorative dentist may be working three rooms at once, doing very technical procedures and working with patients who are extremely nervous. There isn’t time for much education.
For patients with OSA, however, education is imperative. “All of the big studies show that the biggest dropout rate for patients using oral appliances is in the first month,” Demko explains. “So for me it’s about educating the patient to take it slowly, that it’s not going to be easy. And because insurance demands it, they all have 90 days of follow-up in the original fee. If I can get them back for those three months I know I’m already past that big hump where we lose patients to compliance. So, for a dentist who says I’m going to take this course, increase my bottom line by $100,000, it’s not going to happen.”
Demko says the AASDM offers a series of courses for dentists who want to take steps to educate themselves in dental sleep medicine. There’s an introductory course, a full-day clinical course, even podcasts on everything from billing to oral exams. The goal is to guide dentists through the steps necessary to fully understand OSA, but also “to try to explain to them that they can’t go into this for bottom line,” says Demko. “If they go into this for bottom line they will fail. I don’t want to see 25 new patients and none of them have a device made for them. But to have four new patients and all of them have a device made, that’s the difference between understanding what you’re doing, and not.”
Discover more Dentist’s Money Digest® practice management coverage here.
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.