PRF: Here’s Why You Should Consider it for Your Practice
Platelet-rich fibrins promote faster healing and tissue repair by using the patient’s blood. Here’s how it can work in your dental practice.
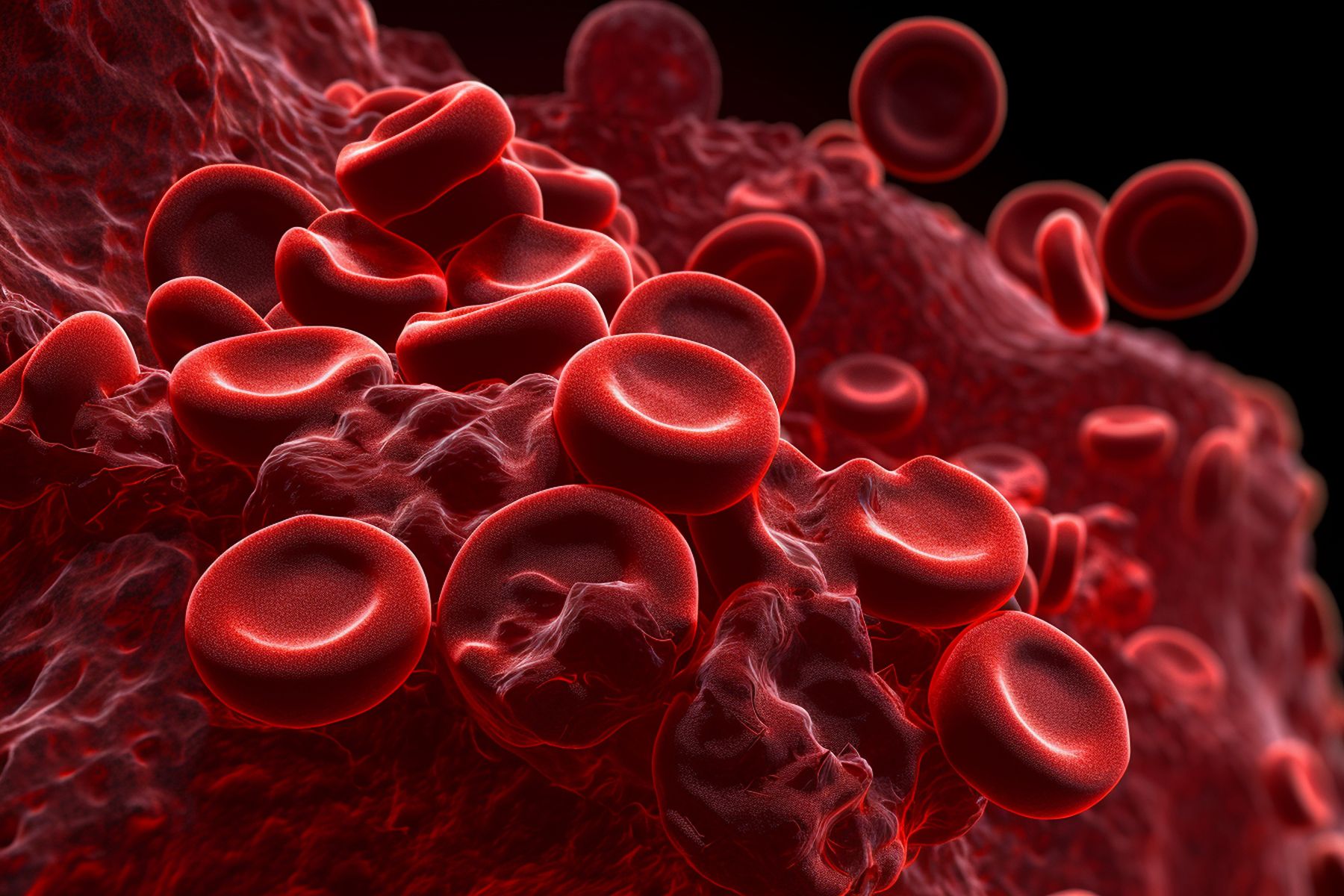
PRF: Here’s Why You Should Consider it for Your Practice | Image Credit: © Катерина Євтехова- stock.adobe.com / AI Generated
For the past 2 decades, dental professionals have been using platelet-rich fibrins (PRF) in oral and maxillofacial surgery. PRF can promote faster healing and tissue repair using the patient’s blood and what that could mean for your practice.
What Is PRF?
PRF is a type of platelet concentrate that helps with healing and recovery. It’s made from the patient’s blood and is easy to produce, making it cost-effective.1
PRF contains leukocytes, platelets, cytokines, and stem cells, which form a strong scaffold that helps the body heal wounds. PRF releases growth factors over time, which help with wound healing but are also good for bone and tissue regeneration. It also helps cells attach and encourages bone cells to grow and develop. PRF doesn’t cause inflammation and can be used alone or with other treatments to help stop bleeding, promote bone growth, and strengthen bones. In addition, it has properties that fight off germs and boost the body’s defenses.
Per the International Journal of Clinical and Experimental Medicine, clinicians can use PRF in the following ways2:
- PRF can act as a resorbable membrane in surgery to guide bone regeneration. It prevents unwanted cells from entering the bone defect while allowing the growth of bone and blood vessels.
- PRF membranes help reshape the alveolar bone and restore gingival tissue, improving mechanical and esthetic properties in natural bone regeneration.
- PRF membranes have shown good results in treating periodontal defects, protecting wounds, and speeding up the healing of hard and soft tissues.
- PRF membranes can seal sinus membrane perforations during maxillary sinus lift procedures.
- PRF membranes aid in wound healing, protect surgical sites, promote soft tissue repair, and attract stem cells when mixed with bone grafts.
- PRF and bone grafts can reduce the volume of bone substitutes needed and improve graft revascularization.
- PRF can speed up bone regeneration in sinus lift procedures when combined with freeze-dried bone allografts, reducing healing time before implant placement.
Per the SELPHYL® System, a platelet-rich fibrin matrix technology, benefits to discuss with patients include the following3:
- Accelerated healing process: PRF therapy harnesses the body’s platelets and growth factors, promoting faster tissue repair and reducing recovery time.
- Reduced risk of allergic reactions: Using the patient’s blood minimizes the risk of allergic reactions or adverse effects, ensuring a safer treatment experience.
- Enhanced tissue healing support: PRF therapy stimulates collagen production and promotes the formation of new blood vessels, leading to robust and sustainable tissue healing support.
- Long-lasting results: PRF therapy targets the condition’s underlying cause, offering more sustainable results than temporary relief methods.
- Versatile applications: PRF therapy shows successful outcomes across various medical and esthetic fields, including orthopedics, dentistry, and dermatology.
- Minimized downtime: PRF therapy typically allows patients to resume regular activities sooner, minimizing disruption to daily life.
Autologous Platelet Concentrations
There have been several generations of autologous platelet concentrations. PRF is the second generation, preceded by platelet-rich plasma (PRP). The journal Decisions in Dentistry provides a helpful summary of the generations, as follows4:
First Generation: PRP
- This involved adding an anticoagulant to venous blood and 2 centrifugations (soft and hard spins) to obtain concentrated PRP.
- The clinical protocol was cumbersome, and the use of anticoagulants and bovine serum posed a risk of cross-contamination.
Second Generation: PRF
- PRF was developed to address PRP’s limitations.
- Leukocyte-PRF (L-PRF), or Choukroun PRF, was introduced using a single centrifugation without added anticoagulants or bovine serum.
- The fibrin aspect provides better scaffolding, similar to a natural blood clot.
- PRF contains platelets, lymphocytes, monocytes, stem cells, granulocytes, and growth factors.
- Advanced platelet-rich fibrin formulations were later introduced, using lower centrifugation forces, which resulted in increased platelets and neutrophilic granules.
Recent Developments:
- Injectable platelet-rich fibrin was developed, involving 1 centrifugation cycle at a lower speed.
- Due to the low centrifugation speed, it contains larger quantities of leukocytes and plasma proteins.
Advantages and Disadvantages of PRF
Like anything in dental or medical procedures, there are tradeoffs with PRF. According to a 2021 study published in the journal Open Medicine, PRF has advantages and disadvantages, which include1:
Clinical Advantages of PRF:
- It is made from the patient’s blood.
- Requires minimal manipulation of blood and no additional chemicals.
- There is no need for bovine thrombin, as the fibrin naturally forms.
- It contains growth factors, leukocytes, and cytokines that aid in healing.
- Releases growth factors over an extended period compared to other platelet concentrates.
- The PRF membrane is highly flexible and elastic.
Clinical Disadvantages of PRF:
- The success of PRF preparation depends on how quickly blood is handled.
- PRF membrane should be used immediately as its structure changes over time.
- PRF membrane storage is impossible due to the risk of contamination and dehydration.
- A limited quantity of PRF is available as it comes from the patient’s blood, making it unsuitable for general surgery.
Should You Try PRF in Your Practice?
Incorporating PRF into treatments has many clinical and patient benefits. Is it the right thing for your practice?
International speaker Ankur Gupta, DDS, a private practice general dentist near Cleveland, Ohio who uses the treatment, says yes. Dr Gupta, a member of the Dental Products Report Editorial Advisory Board, is part of the advocates for PRF based on how it works in his practice, particularly regarding socket preservation.
Dr Gupta says most dentists feel comfortable pulling teeth if a patient needs an extraction. However, if dentists don’t do anything to preserve the socket, bone loss will occur, either vertical or buccolingual bone or both. Dr Gupta explains that pulling the tooth without considering how to prevent this bone loss will lead to long-term inconvenience for a future dental implant or even dentures.
“What we’ve done in this situation is set the patient up for guaranteed bone loss. It’s our responsibility to at least ask the patient whether we can do something to prevent this inevitable bone loss,” Dr Gupta says, adding that most of his patients say yes when presented with an option to preserve bone.
However, traditional socket preservation is technique sensitive. Using bony particulate and securing a membrane on top is challenging for dentists, including Dr Gupta. He admits he was reluctant to perform traditional socket preservations because he didn’t love his results. Therefore, he was enthusiastic about this new option when he learned about PRF.
“The most valuable thing about using the patient’s blood as a substrate for grafting is that it is much more user-friendly. Anybody can graft using PRF because the actual tissue has the same consistency as gingiva,” he says. “It behaves the way gums behave, and you can stick a needle through it the way you stick a needle through gum.”
Also, Dr Gupta appreciates that because the PRF is made from the patient’s blood, it will be more biocompatible, help the wound heal faster, and have fewer complications. Dr Gupta says that anyone can adopt the PRF procedure in their practice. The most intimidating part is drawing blood.
“By taking that extra step to draw some blood, you are setting yourself up for a much easier procedure and more predictability,” he says.
Moreover, clinicians can take the plasma, another by-product of spinning the patient’s blood to create PRF, and mix it with the bony particulate. The consistency is similar to gelatin, making it easier to work with because it handles like materials clinicians are comfortable using.
Another benefit of implementing PRF is that taking a tissue graft from the patient’s palate in attachment loss cases is only sometimes necessary. The PRF can be the graft, which is far less painful and inconvenient for the patient.
“Getting a palate graft is painful,” Dr Gupta says. “This option mitigates the need for that, which is pretty cool.”