Updated: New research suggests a link between gum disease and COVID-19
A new study suggests a link between gum disease and respiratory failure in COVID-19 patients.
Emerging research has suggested a there’s a connection between gum disease and SARS-CoV-2, according to a new report, “The Mouth COVID Connection (MCC).” The review study, which has been accepted for publication for the October 2020 issue of the Journal of the California Dental Association (JCDA), suggests that hospitalized coronavirus patients with prior underlying gum disease can be at higher risk for respiratory failure.
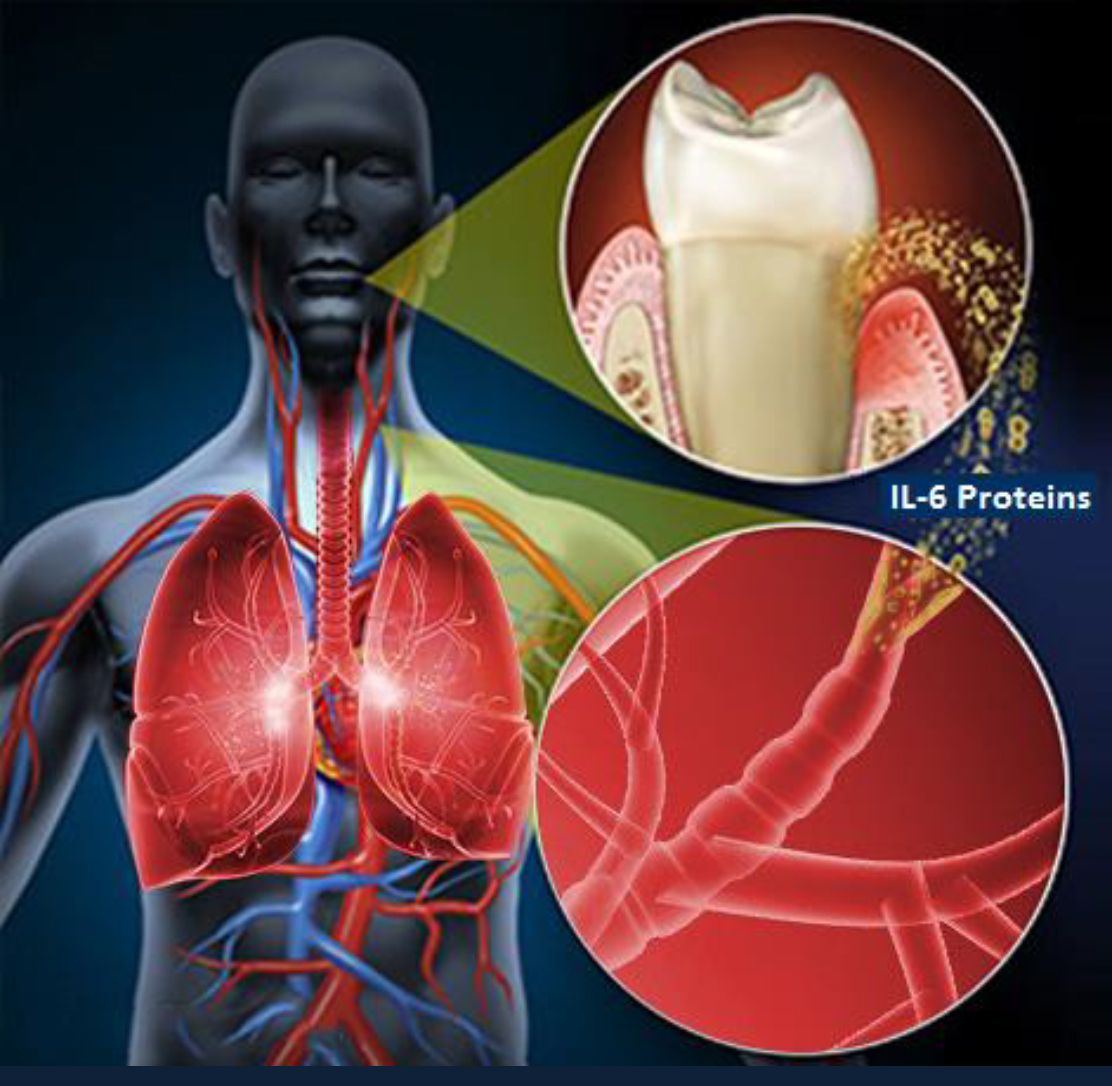
The MCC study suggests a link between the bacteria in inflamed gums and bone loss—symptoms of chronic periodontitis—and COVID-19 complications. Researchers suggest that patients with high levels of IL-6 (interleukin), a harmful protein that is elevated in gum disease, can be at greater risk of suffering life-threatening respiratory problems. A critical study in Germany tested COVID-19 patients for the IL-6 protein while they were hospitalized and determined that patients that presented high Il-6 levels were more likely to need a ventilator to breathe.
The study was conducted by Dr. Shervin Molayem, a dental surgeon based in Los Angeles and founder of the UCLA Dental Research Journal, and Dr. Carla Pontes, a scientist and healthcare researcher in South Africa.
Drs. Molayem and Pontes’ study suggests that patients with bad gums are at risk of generating harmful levels of IL-6 proteins that spread to their lungs. When combined with the SARS-CoV-2 virus, it can contribute to a life-threatening respiratory crisis.
“Gum disease has been linked to other breathing ailments, including pneumonia and chronic obstructive pulmonary disease (COPD), so it seems biologically possible to COVID-19 respiratory problems,” Dr. Molayem said. “The discovery of the protein’s devastating, life-threatening impact to patients once they’re hospitalized provided by the German study made us think of how gum disease could also contribute to high IL-6 levels."
The German study determined that hospitalized COVID-19 patients who had IL-6 levels above 80pg/ml were 22 times more likely to suffer from acute respiratory problems and placed on a ventilator compared to patients with IL-6 levels below 80pg/ml. MCC researches urge anyone concerned they have gum disease to schedule a dental appointment as soon as possible, since several studies show that gum disease can lead to high IL-6 levels.
An analysis of the 153,000 Americans who have died since the first cases were reported highlights a potential role researchers believe gum disease has played—and continues to play—in the pandemic’s rising death toll. Elderly patients—particularly those with immune-compromising, underlying conditions, such as diabetes or cardiovascular disease—are more likely to succumb to life-threatening COVID-19 emergencies, including respiratory failure. MCC researchers say the same demographic is more likely to suffer from chronic gum disease than any other age or demographic.
Researchers hope these findings from their review compel nursing homes to implement a dental screening protocol that will help determine which patients are more vulnerable to gum disease and elevated IL-6 protein levels. They are also urging hospitals and Emergency Room doctors who admit COVID patients to consider gum disease as a hidden source of inflammation.
Researchers say periodontal disease is the most under-diagnosed ailment in dentistry and they urge those who think they may have periodontitis to get treatment as soon as possible.
“As the death toll keeps climbing, the CDC now predicts the virus will be among the leading causes of death in the United States, just behind heart disease and cancer,” said Dr. Molayem. “Periodontitis can make it even deadlier, if you’re worried that you may have gum disease, your next trip to the dentist may actually save your life.”
The study will be published in the October issue of JCDA. The full report can be read at mouthcovidconnection.com.
Study Shows Dental Opioid Prescribing Went Up During COVID-19 Pandemic
November 6th 2023A new study demonstrates that dental opioid prescribing increased during the peak of the COVID-19 pandemic, reinforcing the importance of non-opioid pain management solutions even during global health emergencies.