New Report Finds Millions May Lose Dental Coverage Due to Redetermination
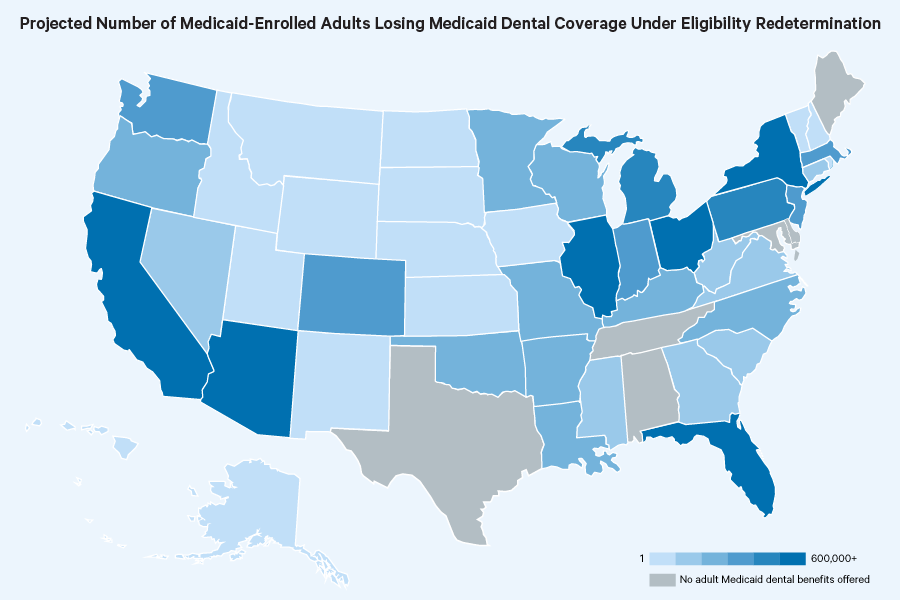
A new report from CareQuest Institute for Oral Health®, a non-profit that focuses on creating a more equitable and integrated oral health system, found that more than 14 million people across the United States may lose dental coverage under the Medicaid redetermination process that began on April 1. Due to the expiration of the national Covid-19 Public Health Emergency on May 11, states are required to start conducting eligibility redetermination and un-enrolling individuals who are considered ineligible from their states’ Medicaid program, according to a press release from CareQuest Institute.
It’s expected that about 15 million people will lose their health coverage as a result. The analysis from CareQuest Institute found that 28% of the country’s adult population currently enrolled in Medicaid may lose dental coverage.
“This new analysis illustrates the concerning impact that the Medicaid redetermination process will have on oral health equity for millions of people across our nation, especially in some of the most marginalized populations,” CareQuest Institute for Oral Health CEO and president Myechia Minter-Jordan, MD, MBA, said, according to the organization’s statement. “We cannot walk back the incredible progress made to strengthen Medicaid dental coverage and connect more people with care in recent years. Access to oral health is critical to good overall health and well-being.”
As dental coverage is lost, many will seek coverage from the private market or through other programs, the press release reads. However, there is no certainty that those who lose Medicaid coverage will be able to find or afford coverage that includes dental benefits. This gap will likely have a greater impact on families of lower income and people of color, according to CareQuest Institute.
How Dentists Can Help Patients Navigate Unforeseen Dental Care
December 12th 2024Practices must equip patients with treatment information and discuss potential financing options before unexpected dental treatments become too big of an obstacle and to help them avoid the risk of more costly and invasive procedures in the future.