How to use fluoride varnish in patients with ‘meth mouth’
Exploring how fluoride varnish helps practitioners address the complexity of dental problems associated with methamphetamine abuse.

Blackened, rotted, crumbling and broken teeth are just a few of the tell-tale signs that your patient may be using methamphetamine (Fig. 1).
Methamphetamine is a highly addictive and dangerous drug used by approximately 900,000 Americans every year. The composition of the drug, pharmacologic effects and users’ behaviors create a perfect storm for the rapid development of dental decay known as “meth mouth.”
Methamphetamine is manufactured from highly acidic and corrosive ingredients such as battery acid, lithium, ammonium fertilizer and cold medications. When smoked, the acidic ingredients enter the oral cavity and begin to demineralize the enamel. In addition to intense pleasure, methamphetamine users experience less desirable effects, including hypo-salivation, bruxism and gingival recession, all known risk factors for dental decay. Further complicating matters are users’ poor oral hygiene, increased sugar consumption and infrequent dental visits. This perfect storm of acidity, hypo-salivation, poor diet and oral hygiene causes carious destruction of many and sometimes all their teeth.
Fig. 1

When they do present to our dental offices, users are often embarrassed by their drug use, concerned about their unattractive smiles and overwhelmed with dental pain. Similarly, as dentists, we may feel overwhelmed by the magnitude and severity of their dental problems and our own uncertainty about which aspects of treatment (surgical, restorative, prosthetic, prevention) to prioritize and initiate.
Successful treatment of meth mouth patients requires simultaneous strategies to address the issues of substance abuse, pain, enamel demineralization and salivary dysfunction. First, dentists should screen all patients for substance abuse by including questions on the topic during their written and verbal review of patients’ general heath. Dentists should refer patients who report current drug abuse to a local rehabilitation center. Secondly, dentists should provide emergency treatment to alleviate dental pain and infections while avoiding, if possible, the use of opioid medications. Third, dentists should utilize preventive agents such as fluoride varnish to promote enamel remineralization, decrease thermal sensitivity and neutralize salivary acidity in these caries-active patients. The use of fluoride varnishes throughout all phases of care can drastically improve restorative outcomes for meth mouth patients and buy time when multiple appointments are required to treat all the decayed teeth.
Profluorid Varnish, a 5% NaF topical fluoride, is one of VOCO’s top-selling products. It is popular for use among children and adolescents but is often underutilized for adult patients that are caries-active, especially due to methamphetamine use. This varnish provides fluoride release, in excess of 6,000 ppm after just one hour, stimulates enamel re-mineralization and relieves dentinal sensitivity. It is packaged as a single-dose delivery system, takes just minutes to apply and comes in five great flavors (caramel, bubble gum, cherry, mint and melon). Unlike other topical fluorides, Profluorid Varnish is a clear varnish and does not cause any temporary or permanent tooth discoloration. This is a distinct advantage for patients who have teeth blackened from methamphetamine abuse and wish to avoid any further discoloration.
A clinical case will be presented in which fluoride varnish (Profluorid Varnish, VOCO) was used in a patient who presented with a moderate form of meth mouth.
Next: A case presentation

Case presentation
Recently, a 46-year-old patient came into our jail dental clinic for an emergency visit. She was experiencing sharp, throbbing and spontaneous pain in an upper right tooth that had broken about one month prior. The patient was aware of many other broken, chipped and/or decayed teeth. The patient recalled that as a young adult, she saw a dentist regularly and felt “proud of her teeth.” Since then, she had lost her job and dental insurance and had developed Type II diabetes. She now sought dental care only when she was in pain and felt her teeth were “weak” and in ill-repair. The patient reported using methamphetamine for the past 17 years and denied any current drug use.
During the clinical exam, I identified that the patient’s pain was originating from the maxillary right first premolar. This tooth was fractured, had pulpal involvement and a periapical lesion, and was non-restorable (Fig. 2). The patient had generalized decay, gingival recession and attrition throughout her mouth. Although the caries was not blackened, the decay pattern (Class V anterior lesions and coronal fractures) was consistent with methamphetamine abuse (Fig. 3).


Fig. 2 Fig. 3
The patient indicated that she was being released from jail in a month. Of concern was whether the patient would follow up and obtain comprehensive care in a dental clinic, school or private practice. Because of these concerns, I recommended applying a topical fluoride varnish to stimulate remineralization and buy her time in obtaining comprehensive care. After extracting tooth #5 and ensuring hemostasis, I applied Profluorid Varnish to the patient’s teeth (Fig. 4).
Eliminate any excess saliva from the patient’s mouth without over-drying. It is important to have saliva present when applying Profluorid Varnish. The varnish sets on contact with saliva and the saliva serves as a carrier which distributes the fluoride throughout the mouth.
Peel back the cover of the SingleDose blister packet of Profluorid Varnish and use the enclosed brush applicator to gently mix the fluoride so it distributes evenly from the well (Fig. 5).

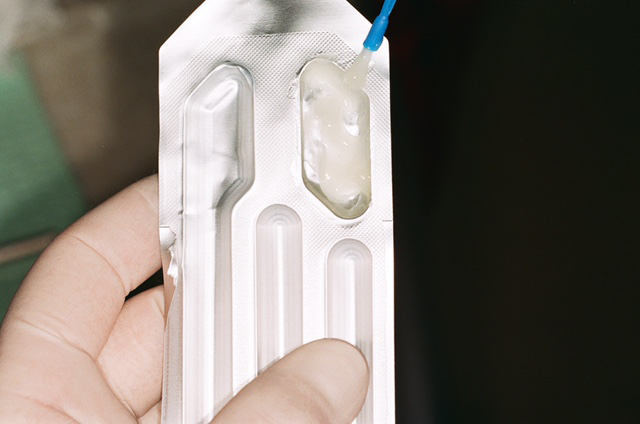
Fig. 4 Fig. 5
Brush Profluorid Varnish onto all the patient’s teeth. In this case, I paid extra attention to the teeth with active carious lesions and demineralized surfaces (Fig. 6). It took less than two minutes to apply.
After fluoride application, instruct the patient to avoid hot or crunchy foods and not to brush or floss for the next four hours.
The patient was seen one week later for a post-operative evaluation. The patient stated that the extraction site was comfortable and my clinical exam revealed that the area was healing within normal limits. She also stated that she had no adverse reactions to the fluoride application and that her teeth felt “stronger and more reinforced” since its application.

Fig. 6
Summary
This case illustrates the challenges faced by both practitioners and patients in addressing the complexity of dental problems associated with methamphetamine abuse. Aside from rampant caries, these users may also experience poverty and incarceration, which limits their ability to obtain comprehensive dental care. As a result, methamphetamine users may over-utilize emergency visits to control their pain and infections. These appointments serve as opportunities for dental professionals to address patients’ chief complaints while simultaneously addressing the broader concern of generalized decay associated with methamphetamine use. This can be accomplished by applying fluoride varnish during these emergency visits as a necessary first step in addressing and repairing the damage caused from methamphetamine abuse.
References
1. Department of Health and Human Services, National Institute on Drug Abuse. NIDA Drug Facts: methamphetamine. https://www.drugabuse.gov/publications/drugfacts/nationwide-trends. Revised February 2017. Accessed: 2017-04-07.
2. Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1- 2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf. Accessed: 2017:04-07.
3. Brown RB, Morisky DE, Silverstein SJ. Meth mouth severity in response to drug-use patterns and dental care access in methamphetamine users. J Calif Dent Assoc. 2013;41:421-428.
4. Baghaie H, Kisely S, Forbes M, Sawyer E, Siskind DJ. A systematic review and meta- analysis of the association between poor oral health and substance abuse. Addiction. 2017;112(5):765-779.