How to achieve esthetic results with direct composites
Why advances in materials and technique are leading to more reliable outcomes.

Although posterior Class I and Class II restorations comprise the majority of direct restorations performed in the average dental practice, anterior composite restorations demand a higher level of esthetic requirements (shade match and surface finish) as these restorations are often the “showcase” work in our patients’ mouths.
This article will address several of the material and technique updates that have improved our ability to more simply and reliably achieve esthetic results with direct composites.
Understanding classifications of composites: a simplified history of filler particles
The dental composite as we know it today was developed in the 1950s by Ray Bowen. At that time, he mixed a bis-GMA resin with silanated 150-micron ground glass filler particles and camphorquinone, a light activator. The most fundamental change between the resin composite of that time and current resin composites is the filler particle. The first major change occurred in the 1970s when submicron (40 nm diameter) round silica particles fabricated from flame pyrolysis were added to the composite to fill in between the large ground glass fillers.1 This formulation was the beginning of the “hybrid” composite as it contained a hybrid of 40 nm fumed silica and 150-micron ground glass. One way to picture these submicron filler particles is to imagine that if the submicron particles were the size of a golf ball, then the 150-micron ground glass fillers would be about the size of a football field.
The next concept in composites was the development of a composite entirely filled with small 40 nm silica particles to take advantage of the polish that can be obtained with small filler particles. To explain this, think of looking out of the window of an airplane. You would not be able to see a divot in the ground the size of a golf ball, but you would definitely notice a football field-sized crater. The same concept applies to filler size when finishing composites.
Unfortunately, adding a filler load of only 40 nm silica particles that is high enough to achieve favorable mechanical properties results in a composite that is too thick to handle in the clinic. Therefore, these fillers were added to resin in a high concentration, completely cured, then crushed into small particles known as prepolymerized filler particles (PPFs). These PPFs were used as the filler particles in microfilled composites. Although microfills achieve a very high polish, these materials fell out of favor due to their inferior mechanical properties, limiting them mostly to anterior restorations.1
The next major development in anterior composites was the nano-filled composite. Unlike the micro-filled composites in which submicron fillers were added as PPFs, nanofilled composites have 5-40 nm silica and zirconia particles clumped together and added as “nano-clusters.” These materials are able to achieve both a high polish and favorable mechanical properties.2
Enhancement of the process of grinding glass fillers has allowed new generations of “hybrid” composites such as micro-hybrid and nano-hybrid composites. These hybrids have smaller and sometimes more homogenously sized ground glass fillers, ranging from a couple microns down to 100 nm.1 In other words, if the original ground glass fillers were the size of a football field, then these glass fillers are closer to the size of a football. They also contain some combination of PPFs, nano-clusters or loose submicron fillers.
These categories are all subjective and it is very confusing for the clinician to differentiate materials based on the information given by the manufacturer. In fact, a researcher dissolved out filler particles from commercially available composites and reported that the sizes of the filler particles were unrelated to the category assigned by the manufacturer.3 In general, current generation composites are either hybrids (containing small ground glass fillers and submicron fillers), micro-filled or nano-filled (Fig. 1). As a rule of thumb, the clinician may ask the manufacturer if its composite has any fillers larger than 500 nm. As the wavelength of visible light ranges from 390-700 nm, particles smaller than this may be visually undetectable after polishing. Additionally, the clinician may consult independent research regarding the gloss, gloss retention and roughness achieved by the composite.
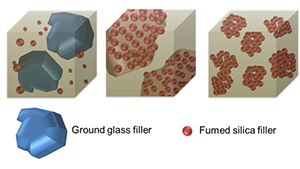
Fig. 1
The chameleon effect: the blending effect of our composite restorations
The “chameleon effect” can more scientifically be defined as a blending effect, the perception that two colors are closer when juxtaposed than when viewed separately. Practically, this means a composite exhibiting a chameleon effect will blend with the surrounding tooth structure. The esthetic-minded dentist will appreciate this trait because it simplifies shade matching, while the business-savvy dentists can appreciate the potential to reduce the number of shades ordered for the clinic. Several attributes of a composite restoration will increase its blending ability such as increasing its polish, decreasing its thickness and using a more translucent composite.4
Many of the composites that are advertised as possessing a chameleon effect are in fact more translucent. For example, Figure 2 shows a 1-mm disc of an A2 shade composite possessing the chameleon effect (Spectra TPH ST, Dentsply Sirona), which is more translucent than the A2 body shade of a reference composite (Filtek Supreme Ultra, 3M ESPE). A conscientious clinician may fear that this translucency is achieved with a lower filler content and reduction in strength. Composite translucency can be changed by modifying the index of refraction of the resin without affecting filler content and preserving strength.5
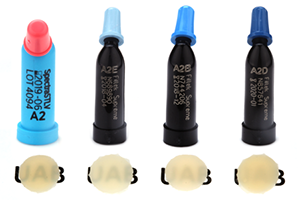

Fig. 2 Fig. 3
More translucent composites that blend well with surrounding tooth structure greatly simplify the process of performing anterior restorations, but they do have their limitations. If placed over a dark tooth preparation, then the underlying tooth structure is more likely to discolor a translucent composite. Also, when translucent composites are used for Class IV restorations in which the lingual wall is absent, the darkness of the oral cavity will manifest as a greying of the restoration (Fig. 3). For these “through and through” Class IV preparations, it is beneficial to use a composite to mimic the opacity of dentin. Several composite systems offer different translucencies of composite. For example, the Filtek Supreme Ultra system offers a dentin shade that is about 60-percent more opaque than the body shade and an enamel shade that is about 30 percent more translucent than the body shade (Fig. 2).6 These dentin and enamel shades can be used to very closely match the natural tooth structure, but it requires a significant amount of experience to correctly achieve the desired effect (Figs. 4-7)
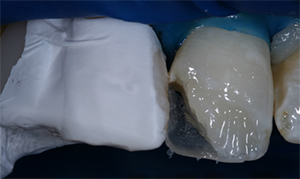
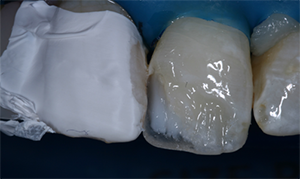
Fig. 4 Fig. 5
Polishers: a key to an esthetic restoration
The polish of a composite restoration can be the key to achieving the esthetic outcome desired by the clinician and patient. But polishing a composite is more than just for the looks. Our patients’ tongues are very sensitive to roughness, with some studies showing that the tongue can detect roughness on the scale of 0.5 microns.7 Composites with roughness values above 0.2 micron are susceptible to plaque accumulation.8 And polishing composites improves their stain resistance.9
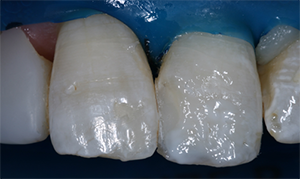

Fig. 6 Fig. 7
Prior to polishing, the restoration is typically finished with either finishing carbides or diamonds. Finishing carbides are typically available as 8-12 bladed (fine), 16-20 bladed (extra-fine) and 30 bladed (ultra-fine). Finishing diamonds are also available in different diamond grit sizes ranging from about 30 microns (fine) to 15 microns (extra-fine) to 8 microns (ultra-fine). A recent study compared the roughness of two different composites when finished with a 20-grit diamond bur and a 30-bladed tungsten carbide bur. There was about a 10-fold increase in roughness using the diamond finishing bur (Ra = 2.5 microns) as compared to the tungsten carbide finishing bur (Ra = 0.25 microns).10
Following the shaping and smoothing of restorations that occurs with a bur, they are then finished and polished. Finishing is the recontouring of a restoration whereas polishing is removing surface irregularities. There are various shapes and formulations of composite finishing and polishing tips (Fig. 8). They all typically contain either aluminum oxide or diamond abrasives. Diamonds are harder and more abrasive than aluminum oxide.

Fig. 8
One of the more popular systems is composed of the Enhance Finishing (first step) and Enhance PoGo Polishing (second step) tips (Dentsply Sirona). They are available in a disk, point and cup. The cups can be used for gingival margins and achieving labial contours, whereas the points can be used to achieve labial contours and polish the lingual of anterior teeth. The Enhance Finishing tips contain larger aluminum oxide particles while the PoGo Polishing tips contain smaller diamond particles (Figs. 9-10). The abrasive particles are embedded in a urethane dimethacrylate binder. This binder allows these tips to finish/polish aggressively and quickly with high pressure and then smooth with lower pressure. The binder will wear away quickly when high pressure is applied during aggressive finishing/polishing, which limits the lifetime of these tips. Other systems with points and cups use rubber-based binders (Optrapol, Ivoclar Vivadent; Jiffy, Ultradent), which will preserve the shape and increase the lifetime of the finisher/polisher, but it does not allow for aggressive finishing/polishing with high pressure.
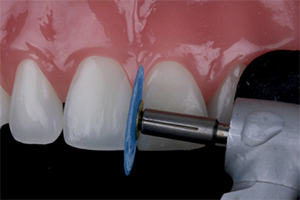
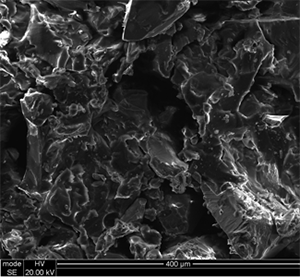
Fig. 9 Fig. 10
The other commonly used tools for finishing and polishing anterior composites are flexible polishing discs (i.e. Sof-Lex Contouring and Polishing Discs, 3M ESPE; FlexiDisc, Cosmedent). These contain aluminum oxide particles of different sizes ranging from 5 microns (super fine) to 14 microns (fine) to 29 microns (medium) to 100 microns (coarse). The medium and coarse discs can finish and recontour the restoration. Several studies have compared the polish achieved with flexible polishing discs to the polishing points, with some studies showing an advantage with the points10 and others with the discs.11 Practically, the advantage of polishing discs in anterior restorations is that these discs are flexible and will often help to create smooth contours of the restoration. They can also adapt to embrasure spaces (Fig. 11).
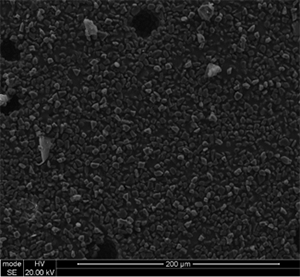
Fig. 11
Some of the newest composite polishers are spiral-shaped (Sof-Lex Diamond, 3M ESPE, DiaComp Feather Lite, Brasseler USA; Footsie Composite Polisher, Komet) (Figs. 12-13). A recent study determined these polishers were able to achieve a smoother surface than several polishing points.12 In the author’s experience, the spiral-shaped polishers will obtain a very high gloss. Due to their shape, however, they will not achieve any finishing, so any gross irregularities should be removed with a finishing bur prior to using these polishers.
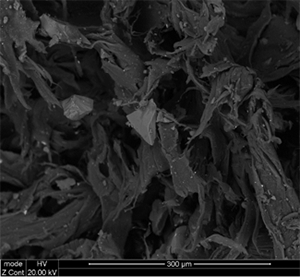
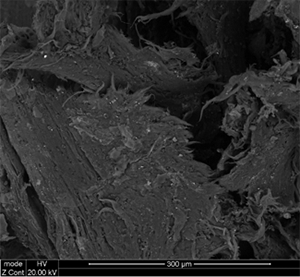
Fig. 12 Fig. 13
The final step in polishing is the application of a polishing paste. The main components include diamond and/or aluminum oxide particles to serve as abrasives with a glycerin-based lubricant. For the application of pastes, buffing polishers are ideal (FlexiBuff, Cosmedent, Goat Hair Brush, Ultradent).
References
1. Ferracane JL. Resin composite--state of the art. Dent Mater. 2011 Jan;27(1):29-38
2. Mitra SB, Wu D, Holmes BN. An application of nanotechnology in advanced dental materials. J Am Dent Assoc. 2003 Oct;134(10):1382-90.
3. Lang BR, Jaarda M, Wang RF. Filler particle size and composite resin classification systems. J Oral Rehabil. 1992 Nov;19(6):569-84.
4. Paravina R, Westland S, Imai F, Kimura M, Powers J. Evaluation of blending effect of composites related to restoration size. Dent Mater 2006;22(4)299-307.
5. Ota M, Ando S, Endo H, Ogura Y, Miyazaki M, Hosoya Y. Influence of refractive index on optical parameters of experimental resin composites. Acta Odontol Scand. 2012 Sep;70(5):362-7.
6. Ryan EA, Tam LE, McComb D. Comparative translucency of esthetic composite resin restorative materials. J Can Dent Assoc. 2010;76:a84.
7. Jones CS, Billington RW, Pearson GJ. The in vivo perception of roughness of restorations. Br Dent J 2004;196(1):42-5; discussion 31.
8. Bollen C, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention retention: a review of the literature. Dent Mater 1997; 13: 258-269.
9. Barakah HM, Taher NM. Effect of polishing systems on stain susceptibility and surface roughness of nanocomposite resin material. J Prosthet Dent. 2014 Sep;112(3):625-31.
10. Daud A, Gray G, Lynch C, Wilson N, Blum I. A randomized controlled study on the use of finishing and polishing systems on different resin composites using 3D contact optical profilometry and scanning electron microscopy. J Dent 2018; 71: 25-30.
11. Gönülol N, Yilmaz F. The effects of finishing and polishing techniques on surface roughness and color stability of nanocomposites. J Dent. 2012 Dec;40 Suppl 2:e64-70.
12. Pala K, Tekçe N, Tuncer S, Serim ME, Demirci M. Evaluation of the surface hardness, roughness, gloss and color of composites after different finishing/polishing treatments and thermocycling using a multitechnique approach. Dent Mater J. 2016;35(2):278-89.
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.