Getting Direct about Indirect Dental Restorative Materials: Why Ceramics and Resins Are Leading Development
We take a look at the different types of indirect dental restorative materials and which ones are likely to be the ones you choose for your next case.
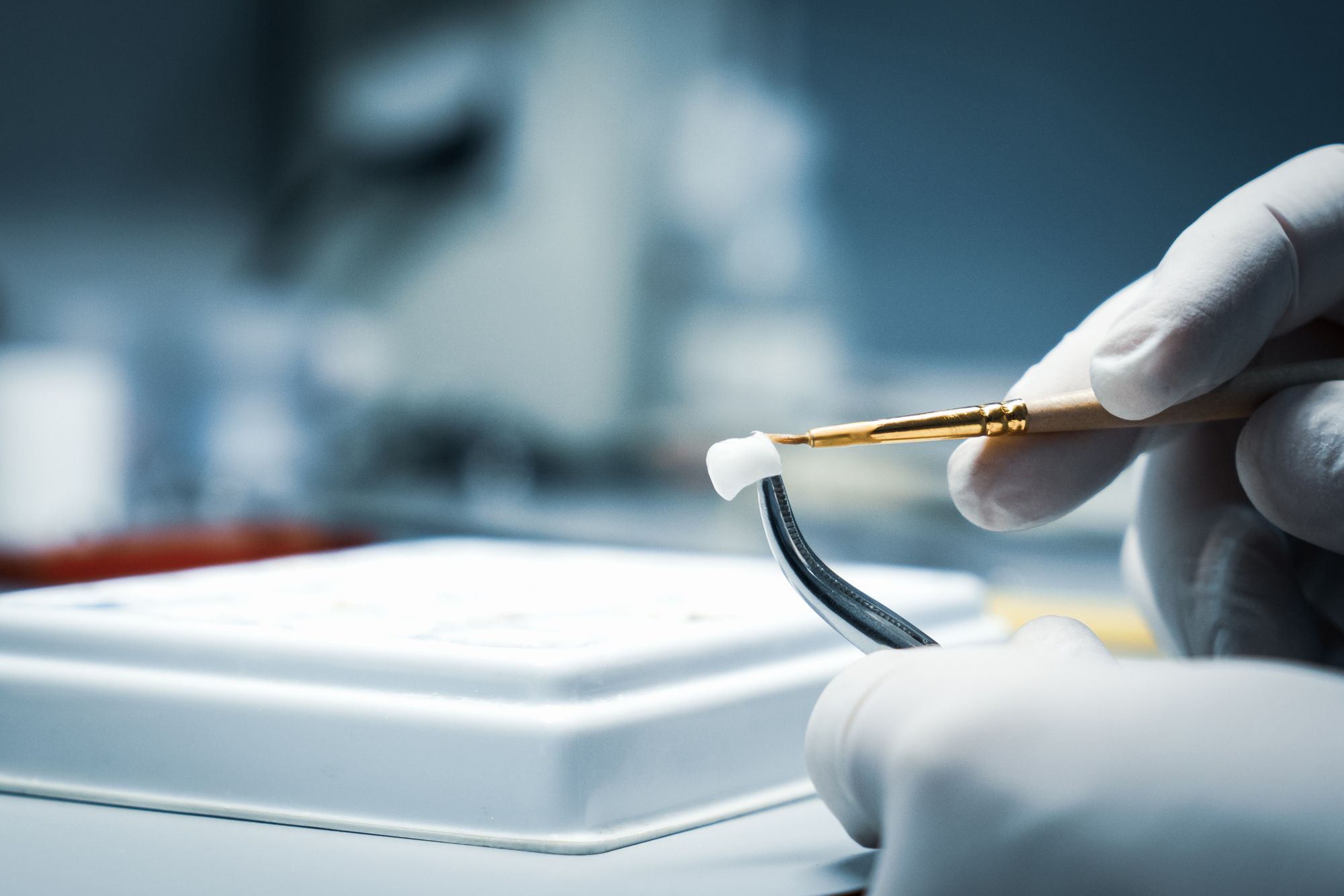
Getting Direct about Indirect Dental Restorative Materials: Why Ceramics and Resins Are Leading Development. Photo courtesy of metr1c/stock.adobe.com.
In the old days, there weren’t a lot of options for replacing indirect restorations. Or maybe there were, if you think all the animals’ teeth in the animal kingdom were an option, or maybe just their tusks. Of course, you could always get human teeth to replace the missing ones in a mouth, provided there had a been a good haul from the poor districts or a giant battle with lots of casualties in a field nearby.
Luckily, we don’t have to resort to such macabre measures these days to restore missing teeth. Several materials exist to fabricate indirect restorations. Whether you choose them, or the lab does, we take a look at the different types of indirect materials and why ceramics and resin composites could be what you choose for your next case.
Different Types of Indirect Restorative Materials
Today’s indirect materials break down into the following categories and usages:1
- High Noble, Noble Alloys: Inlays, onlays, crowns, fixed bridges, and infrastructures
- Base Metal Alloys: bridges crowns and partial dentures
- All-Ceramic: Inlays, onlays, crowns, esthetic veneers
- Resin-Based Ceramic: Inlays, onlays, and long-term temporaries
- Metal Ceramic: Crowns and fixed bridges.
Each indirect material has advantages and disadvantages, indications and contraindications, per the American Dental Association (ADA). There are also 4 considerations about your indirect materials that should go into the materials selection decision: composition, physical and mechanical properties, processing methods, and clinical indications.2 Of course, patients would likely add a fifth consideration, cost.3 (To be fair, many clinicians would, too.)
There are more clinical considerations regarding material choices for an indirect restoration, too. These include things like the tooth location, the amount of tooth that will show when the patient smiles, the position of the patient’s gum, what the tooth needs to do, how much natural tooth remains, and the appearance of the surrounding dentition.4
For example, if you are placing an implant and need to choose a crown material, you would determine what you want the restored tooth to do, the mechanical properties of the material you use and how it will hold up at that position. A temporary crown or restoration to allow the patient’s bone time to heal before placing the permanent one might lead you to select composite-resin. However, if you don’t need a temporary first, you might pick a porcelain-fused-to-metal or an all-ceramic material, like zirconia, instead.5
Of course, you might not choose one at all and let your lab technician partner decide, which is also a great solution. It’s all in how you want to work.
Survival of the Fanciest
The different materials are associated with specific longevity rates. Not surprisingly, gold, and the other metal and metal alloy restorations, have the longest survival rate, with an average of around 20 years, and in some cases double that, and the lowest annual failure rate. Next came, the metal-ceramic crowns, which averaged 10-25 years. Zirconia and feldspathic porcelain (a glass material with a non-crystalline structure) came in at 10 years.6 CAD/CAM materials (single tooth), lithium disilicate or leucite reinforced, glass infiltrated ceramics, and resin composites all had a survival rate of 5 years. There is a comprehensive overview from the ADA on indirect materials if you want to learn more about your choices, use cases, advantage and disadvantages, and survivability and longevity rates.
Ceramics and Resin Composites Are Driving the Indirect Material Development Game
Historically, the choices for indirect restorative materials were a bit easier because of the dearth of options. Clinicians used metals for the restorations because metals were strong and lasted a long time. Even today, after the advent of more esthetic materials than metal, the ADA describes metals, like gold, base metal alloys, and even amalgam as useful restorative materials.7 The ADA’s report from the science and research institute describes high noble alloys (like gold) as “the standard by which other dental materials are judged.”
However, despite the performance of metals like gold, people started wanting tooth-colored restorations, which metal could not deliver, but ceramics could. Unfortunately, ceramic materials could also fracture and couldn’t last as long as the metal restorations did. Regardless of the shortcomings for longevity and strength, materials manufacturers developed many different ceramic materials options from which to choose. These include glass-ceramics, porcelain, and polycrystalline ceramics.8
Porcelain fused-to-metal systems were introduced in the mid-twentieth century. Later in the early 60s, incorporating more leucite crystals into the feldspathic porcelain’s makeup increased the strength of the restorations. The leucite crystals increased the thermal expansion of the porcelain, matching it closer with the metal substrate. This enhancement created strong restorations.9
Early ceramic restorative materials often had clinicians choosing between those that were strong or those that looked good. However, materials science has advanced to the point today that many of dental newer ceramic indirect materials are strong and esthetic. Also, ceramic materials appealed to clinicians because of their biocompatibility and chemical stability.10 Moreover, computer-aided fabrication techniques are advancing all the time, which increased the popularity of all-ceramic indirect restorations. The classes of ceramics for use in CAD/CAM processing are zirconia, glass ceramics, and resin-ceramic composites.11 Zirconia and lithium disilicate are 2 of the most popular all-ceramic materials today.
However, ceramics are not the only tooth-colored options for indirect restorations. There are also the resin-matrix composites, which are known for their easy-to-manipulate characteristics. However, indirect resin-matrix composites differ from direct restoration composites because these materials often have higher filler loads and higher degrees of polymerization than the direct versions. Also, indirect restorative composites have fewer problems with polymerization shrinkage since they are cured outside the patient’s mouth. In addition, the CAD/CAM blocks of it are more biocompatible than their direct composite counterparts because manufacturers’ use different resins for the block versions. Plus, these indirect CAD/CAM composite versions demonstrate more resistance to degrading and leaking, have more flexibility during chewing forces, and are less abrasive to opposing dentition. However, they also tend to have lower flexural strength and fracture toughness. These indirect composites are usually made of urethan dimethacrylate (UDMA), triethylene glycol dimethacrylate (TEGMDA), or Bis-GMA bisphenol A-glycidyl methacrylate for the matrix, and silica, silica-based glasses, glass-ceramics, zirconia, or zirconia-silica ceramic for the fillers.12
Ceramics and resin-based composites tend to be popular for indirect restorations because of their composition and characteristics. For example, all-ceramic indirect restorations are an excellent choice when you are placing crowns, inlays, onlays, veneers and bridges.13 Resin composites have been widely recommended as long-term provisional restorations.14 Also, some evidence suggests that resin composites can offer a better-looking material for posterior indirect restorations, and in some cases, might offer a better solution than ceramics for some patients’ crowns, particularly to absorb chewing stresses in implants when the patient has poor periodontal structures supporting the restoration.15
For full-arch cases, however, some dentists prefer all-ceramic materials, like zirconia, to resin composites. In these high-priced, full-mouth restorative treatments, clinicians favor the predictable mechanical performance of the ceramics over ceramic-, acrylic-, and resin-metal alloy prostheses. Moreover, improvements to the material compositions in the last few years have created all-ceramic materials that are strong like their predecessors, but much more esthetic. Some other benefits noted are increased accuracy, decreasedveneering porcelain and the need for minimal occlusal adjustments. Also, using a full occlusal monolithic framework and minimal facial cutback can reduce the chipping of the veneered porcelain.16
Things have changed for the better with indirect restorative materials, when you consider what was available over the course of history. All of today’s indirect materials have strengths and weaknesses, but the rising popularity of CAD/CAM systems and milling for chairside or lab production of indirect restorations is likely to continue development in the direction of all-ceramic and composite resin materials.
References
Materials for Indirect Restorations. Ada.org. Published 2021. Accessed January 31, 2022. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/materials-for-indirect-restorations.
Materials for Indirect Restorations. Ada.org. Published 2021. Accessed January 31, 2022. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/materials-for-indirect-restorations.
Larson J. Dental Crown Types, Procedure, When It's Done, Cost, and Aftercare. Healthline. Published 2019. Accessed February 11, 2021. https://www.healthline.com/find-care/articles/dentists/dental-crown#types.
Larson J. Dental Crown Types, Procedure, When It's Done, Cost, and Aftercare. Healthline. Published 2019. Accessed February 11, 2021. https://www.healthline.com/find-care/articles/dentists/dental-crown#types.
Larson J. Dental Crown Types, Procedure, When It's Done, Cost, and Aftercare. Healthline. Published 2019. Accessed February 11, 2021. https://www.healthline.com/find-care/articles/dentists/dental-crown#types.
Jones, PhD, FIM, CCHem. FRSC, FBSE D. CDA-ADC Journal. Cda-adc.ca. Published 1998. Accessed February 3, 2022. https://www.cda-adc.ca/jcda/vol-64/issue-9/648.html.
ADA Council on Scientific Affairs. Direct and indirect restorative materials. J Am Dent Assoc. 2003;134(4):463-472. doi:10.14219/jada.archive.2003.019
Materials for Indirect Restorations. Ada.org. Published 2021. Accessed January 31, 2022. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/materials-for-indirect-restorations.
Jones, PhD, FIM, CCHem. FRSC, FBSE D. CDA-ADC Journal. Cda-adc.ca. Published 1998. Accessed February 3, 2022. https://www.cda-adc.ca/jcda/vol-64/issue-9/648.html.
Jones, PhD, FIM, CCHem. FRSC, FBSE D. CDA-ADC Journal. Cda-adc.ca. Published 1998. Accessed February 3, 2022. https://www.cda-adc.ca/jcda/vol-64/issue-9/648.html.
Materials for Indirect Restorations. Ada.org. Published 2021. Accessed January 31, 2022. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/materials-for-indirect-restorations.
Materials for Indirect Restorations. Ada.org. Published 2021. Accessed January 31, 2022. https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/materials-for-indirect-restorations.
Warner B. COMPARE INDIRECT AND DIRECT RESTORATIVE MATERIALS IN DENTISTRY. Blog.ddslab.com. Published 2022. Accessed February 1, 2022. https://blog.ddslab.com/indirect-and-direct-restorative-materials.
Larson J. Dental Crown Types, Procedure, When It's Done, Cost, and Aftercare. Healthline. Published 2019. Accessed February 1, 2022. https://www.healthline.com/find-care/articles/dentists/dental-crown#types.
Nandini S. Indirect resin composites. J Conserv Dent. 2010;13(4):184-194. doi:10.4103/0972-0707.73377
Winstead, CDT M, Arce, DDS C. Technique: Fabricating full arch implant prosthesis. Dental Products Report. Published 2017. Accessed February 1, 2022. https://www.dentalproductsreport.com/view/technique-fabricating-full-arch-implant-prosthesis.
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.