Genetic Insights and Advanced Treatments in Peri-Implantology: A Comprehensive Approach to Peri-Implant Health
In the first installment of "Perio Power for the Hygienist", the author explores the genetic underpinnings, preventive strategies, and innovative treatments for peri-implant diseases in modern periodontology.
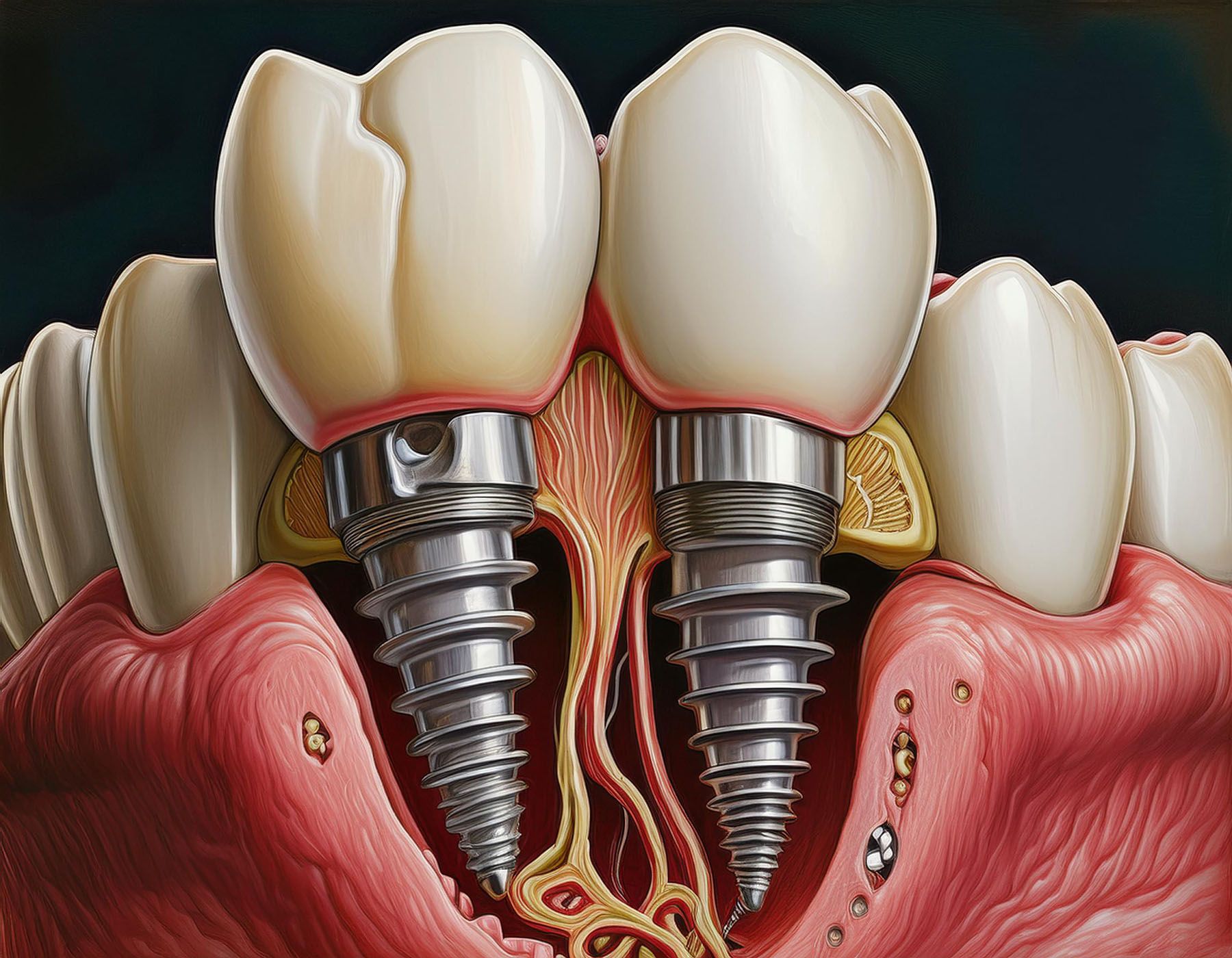
Genetic Insights and Advanced Treatments in Peri-Implantology: A Comprehensive Approach to Peri-Implant Health | Image Credit: © Generated with Adobe Firefly
Preface
This is the first in a series of dental hygiene articles—Perio Power for the Hygienist—from the American Academy of Periodontology (AAP). Flavia Pirih, DDS, PhD, presented at the American Academy of Periodontology 109th Annual Meeting in 2023 with a focus on the genetic components of periodontitis and peri-implantitis, the increasing prevalence of dental implants, and the necessary preventive and treatment measures for maintaining peri-implant health. Her lecture is a comprehensive guide for periodontists and dental hygienists alike, providing valuable insights into the complexities of peri-implant diseases and the importance of an evidence-based approach to treatment and maintenance. Her emphasis on genetic research opens new avenues for personalized patient care and highlights the evolving nature of periodontology in the era of advanced dental implants.
Perio Power for the Hygienist is a series of articles from the AAP focusing on key topics in the field of periodontics.
Introduction to Peri-Implant Diseases
While dental implants have revolutionized restorative dentistry by improving function, esthetics, and phonetics, they come with their own set of challenges. The significant rise in implant placements underscores the need to manage peri-implant diseases effectively.
The increasing popularity of dental implants has led to a decrease in other restorative procedures such as endodontic treatments and prosthetic placements. Data illustrate this trend, noting that the global dental implant market was valued at approximately $4.6 billion in 2022, with an estimated 500,000 to 800,000 implants placed annually in the United States alone. This rise emphasizes the importance of understanding the complications associated with implants, particularly peri-implant diseases.
Peri-Implant Health
Peri-implant health is characterized by the absence of inflammation, redness, swelling, and profuse bleeding. Establishing baseline measurements for probing depths and radiographic assessments at the time of implant placement is crucial. Healthy peri-implant pockets can be up to 5 mm deep, provided there is no inflammation or bleeding.
Initial radiographic assessments should be conducted when healing abutments are placed, and follow-up radiographs are essential to monitor any changes in bone levels. Bone remodeling typically occurs within the first-year post-implant placement, with bone loss not exceeding 2 mm during this period being considered normal.
Distinguishing between normal and pathological conditions is necessary, particularly in cases where pockets deeper than 5 mm are present but show no signs of inflammation or bleeding. Such conditions can still be classified as healthy if proper baseline measurements and consistent monitoring are maintained.
Peri-Implant Mucositis and Peri-Implantitis
Peri-implant mucositis is the precursor to peri-implantitis and is marked by inflammation, redness, swelling, and bleeding on probing without bone loss. Identifying and treating mucositis early is crucial to prevent progression to peri-implantitis, which involves both inflammation and progressive bone loss around the implant. Studies show significant rates of peri-implant mucositis and peri-implantitis among implant patients. Key risk factors include poor plaque control, smoking, and excess cement.
Peri-implantitis, in contrast to mucositis, is associated with radiographic evidence of bone loss in addition to clinical signs of inflammation. Peri-implantitis can progress rapidly if not managed promptly, leading to severe bone loss and potential implant failure. Data indicate that while the prevalence of peri-implantitis at the implant level is around 8%, it can be as high as 14% at the patient level.
Implants require as much care and monitoring as natural teeth, if not more, to prevent diseases like peri-implantitis. The presence of soft tissue inflammation and radiographic bone loss are critical markers for diagnosing peri-implantitis.
Risk Factors and Preventive Measures
Plaque accumulation is the primary etiological factor for both peri-implant mucositis and peri-implantitis. The importance of rigorous oral hygiene practices and regular maintenance visits is emphasized. The impact of smoking and diabetes on peri-implant health is also discussed, noting that both conditions exacerbate inflammatory responses and increase the risk of peri-implant diseases.
Smoking is highlighted as a significant risk factor, with data indicating that smokers have a higher prevalence of peri-implant diseases compared to non-smokers. Studies show that smokers are more likely to experience crestal bone loss and peri-implantitis. Confounding variables in studies related to smoking, such as self-reporting inaccuracies and the presence of other risk factors like periodontitis, are also discussed.
Diabetes is another critical risk factor. Patients with uncontrolled diabetes are more susceptible to peri-implant diseases due to impaired immune responses and delayed healing. Animal model studies demonstrate the exacerbating effects of diabetes on peri-implantitis, showing faster and more severe bone loss in diabetic conditions.
Preventive measures are essential for managing these risks. Thorough patient education on maintaining oral hygiene, regular professional cleanings, and addressing systemic conditions like diabetes and smoking cessation is crucial. Designing prosthetic superstructures that allow for easy cleaning to prevent plaque accumulation is also highlighted as an important preventive measure.
Treatment Protocols
Both non-surgical and surgical treatment protocols for peri-implant diseases are outlined. Non-surgical treatments include mechanical debridement using curettes (plastic, carbon, or titanium), ultrasonic scalers, and air polishing devices. The goal is to remove biofilm and reduce bacterial load. Non-surgical treatments can be effective in managing peri-implant mucositis but are often insufficient for peri-implantitis, which typically requires surgical intervention.
Non-surgical debridement focuses on disrupting and removing the biofilm to reduce inflammation and bacterial load. The use of plastic curettes to minimize damage to the implant surface is recommended, although plastic debris can sometimes be left behind. Ultrasonic scalers and air polishing devices, such as those using glycine powder, are also recommended for their efficacy in biofilm removal and minimal implant surface damage.
Surgical Intervention
For peri-implantitis, surgical interventions aim to clean the implant surface, reduce pocket depths, and regenerate lost bone where possible. Resective surgery focuses on minimizing the defect and improving access for oral hygiene, while regenerative surgery aims to rebuild lost bone and support tissues.
The author presents several case studies to illustrate these approaches. One case involves a patient with significant peri-implantitis who underwent resective surgery to reduce pocket depths and remove inflamed tissue. The outcome showed reduced inflammation and improved implant stability, although aesthetic results were not ideal.
Related reading: Chicago Midwinter Meeting Plays Host to AAP’s Perio Power Hour
In another case, regenerative surgery was performed using bone grafts and membranes to encourage bone regrowth around the implant. In this case, I highlight the importance of selecting appropriate cases for regenerative procedures, noting that contained defects and aesthetic considerations are key factors in decision-making.
Case Studies and Practical Implications
I share several case studies to illustrate the practical application of the principles discussed. These cases highlight the importance of thorough diagnosis, tailored treatment plans, and the critical role of patient compliance in maintaining peri-implant health.
One notable case involved a young patient with aggressive periodontitis who lost all her teeth by the age of 30. Despite undergoing full-mouth reconstruction with implants, she developed severe peri-implantitis within 2 years. I suggest that genetic predispositions may play a significant role in such aggressive cases and emphasizes the need for careful patient selection and monitoring.
Another case study involves a patient with poor oral hygiene and multiple implants. The patient was initially treated with non-surgical debridement, but due to the severity of the condition, surgical intervention was required. I performed a combination of resective and regenerative procedures, ultimately achieving a stable and healthy peri-implant environment.
Genetics and Periodontitis
The genetic underpinnings of periodontitis sheds light on how genetic factors contribute to the susceptibility and progression of this chronic inflammatory disease. Periodontitis is a multifactorial condition influenced by a complex interplay of microbial, environmental, and host factors, among which genetics play a crucial role.
Genetic predisposition accounts for a significant proportion of the variability in the individual response to periodontal pathogens. Studies have identified several genetic polymorphisms that are associated with an increased risk of developing periodontitis. For instance, variations in genes encoding cytokines, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α), have been linked to heightened inflammatory responses and tissue destruction in periodontal disease. These cytokines are critical in the regulation of the inflammatory process, and their overexpression can lead to excessive tissue breakdown and bone resorption.
Genetic variations can influence the function of immune cells, such as neutrophils and macrophages, which are essential in combating periodontal pathogens. Defects in neutrophil function, for example, have been observed in certain genetic disorders, leading to severe forms of periodontitis. Additionally, polymorphisms in genes related to the innate immune system, such as toll-like receptors (TLRs), can alter the host’s ability to recognize and respond to microbial invaders, thereby affecting disease susceptibility and progression.
Genetics and Peri-Implantitis
Similar to periodontitis, genetic factors significantly influence the risk and progression of peri-implant diseases. Peri-implantitis, characterized by inflammation and bone loss around dental implants, shares several pathophysiological mechanisms with periodontitis, including the host’s genetic response to bacterial colonization.
Genetic polymorphisms in inflammatory cytokines and immune regulatory genes also play a critical role in peri-implantitis. The same genetic variations that predispose individuals to periodontitis can similarly affect their susceptibility to peri-implantitis. For example, polymorphisms in the IL-1 gene cluster have been associated with increased peri-implant bone loss, suggesting a common genetic basis for these two conditions.
Genetic screening for specific polymorphisms could potentially identify individuals at higher risk for peri-implantitis, allowing for personalized preventive and therapeutic strategies. This approach aligns with the broader trend towards precision medicine, where treatments and preventive measures are tailored to the genetic profile of the individual.
Genetic Research and Clinical Implications
Ongoing research is needed to further elucidate the genetic factors involved in periodontitis and peri-implantitis. Advances in genomic technologies, such as genome-wide association studies (GWAS) and next-generation sequencing (NGS), have opened new avenues for identifying genetic variants associated with these conditions. These technologies enable researchers to analyze the entire genome and identify novel genetic markers that could contribute to disease susceptibility.
The integration of genetic research into clinical practice has significant implications for the management of periodontitis and peri-implantitis. By identifying genetic risk factors, clinicians can develop more targeted and effective treatment plans. For instance, patients with a genetic predisposition to heightened inflammatory responses may benefit from more aggressive anti-inflammatory therapies or closer monitoring to prevent disease progression.
Additionally, understanding the genetic basis of these diseases can lead to the development of new therapeutic targets. Future treatments could involve modulating specific genetic pathways to reduce inflammation and promote tissue regeneration. This could include gene therapy approaches or the use of small molecules to specifically target the inflammatory processes driven by genetic variations.
Future Directions
My research at UCLA is pioneering in exploring the genetic components of periodontitis and peri-implantitis. Preliminary findings in ongoing studies involving animal models suggest that genetic predispositions can significantly influence the severity and progression of peri-implant diseases.
Data from animal studies where different strains of mice were used to study the genetic variability in response to peri-implant diseases have shown significant differences in bone loss and inflammatory responses, suggesting that genetics play a crucial role in disease progression.
Understanding the genetic basis of peri-implant diseases could lead to more personalized treatment approaches. This research aims to identify specific genetic markers that predispose individuals to peri-implantitis, which could eventually allow for tailored preventive and therapeutic strategies.
Conclusion
In conclusion, preventive measures, including meticulous oral hygiene, regular maintenance, and patient education are critically important. The author calls for a balanced approach in clinical practice, where the benefits of dental implants are weighed against the potential risks of peri-implant diseases. I also want to underscore the necessity for continuous research and innovation in understanding and managing peri-implant health, ultimately aiming to improve patient outcomes and longevity of dental implants.
Overall, I encourage dental professionals to adopt a proactive stance in managing peri-implant health, emphasizing prevention, patient education, and the integration of genetic insights into clinical practice. By doing so, dental professionals can enhance the longevity and success of dental implants, ensuring optimal patient outcomes.