Enhancing Efficiency in the Dental Treatment Room
There are many safe and effective ways to boost efficiency in the dental treatment room.
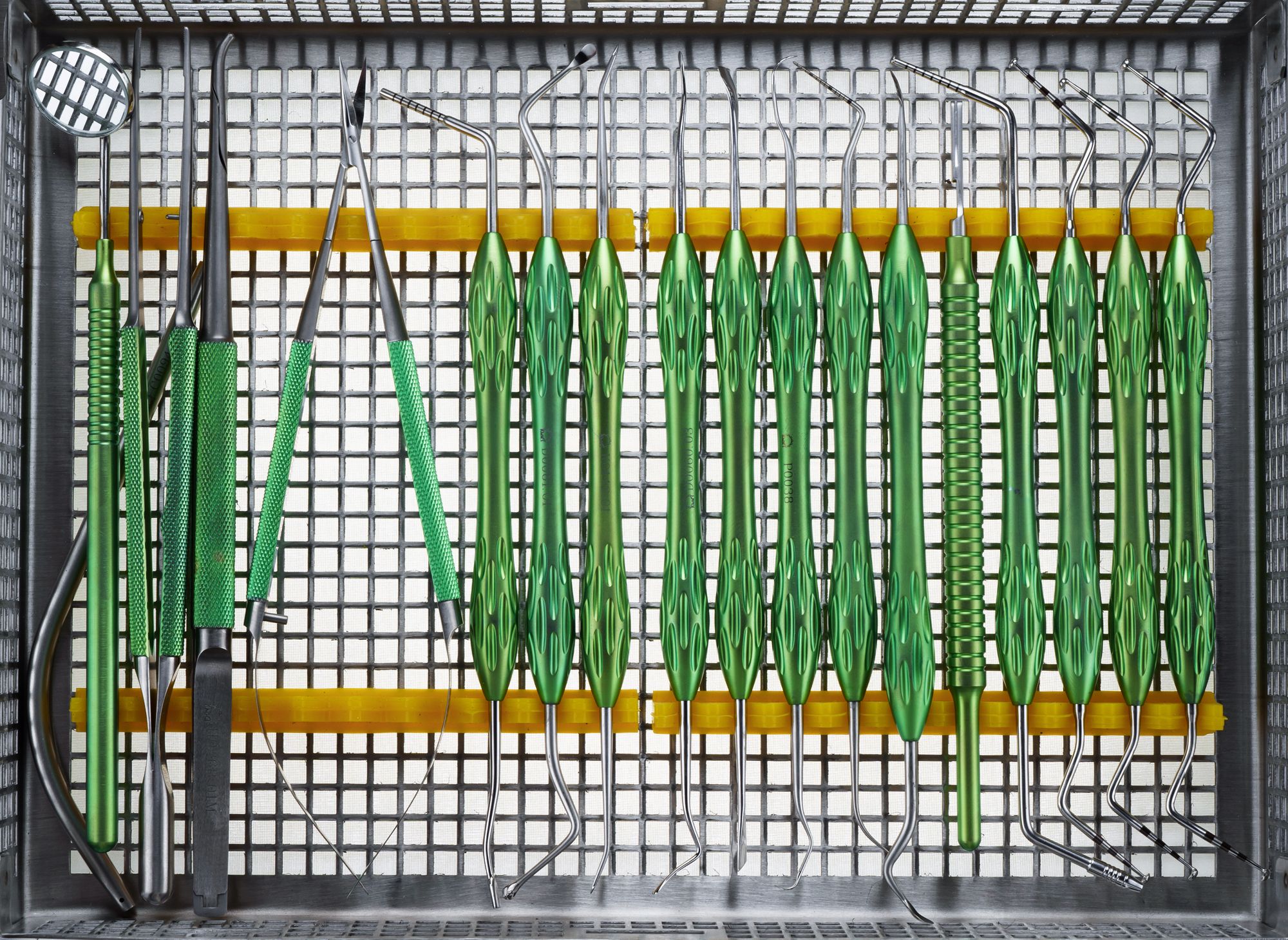
Enhancing Efficiency in the Dental Treatment Room. Photo courtesy of Dental Pro Content/stock.adobe.com.
In the middle of a home improvement project, Marge Simpson scrutinizes Homer Simpson’s questionable method, leading to his defensiveness.
“Listen,” he says. “Do you want the job done right or do you want it done fast?”
While no one is comparing dental professionals to Homer Simpson, the good news is that infection control tasks can be done both safely and efficiently – it just requires some forethought.
With the help of infection prevention consultants and podcasters The Compliance Divas, we look at sources of enhancing efficiency throughout the dental practice. Part 1 examined efficiencies in the sterilization area. In this Part 2, we will look at efficiencies in the treatment room.
The Compliance Divas — Mary Govoni, Leslie Canham, Olivia Wann, and Linda Harvey (thecompliancedivas.com) — are a group of consultants with a weekly podcast covering current topics such as infection prevention and control, Occupational Safety and Health Administration (OSHA) and Health Insurance Portability and Accountability Act (HIPAA) compliance for dentistry. They discuss the latest regulatory information, answer frequently asked questions, and give suggestions for dental practices to make compliance easy and sustainable.
Cassettes and Instrument Management Systems
A lot of inefficiencies can be mitigated through optimized instrument handling. A great way to simplify, streamline, and organize is by using cassettes.
“Cassettes are becoming much more popular, because practices are seeing how efficient they are,” infection prevention speaker, author, and consultant Mary Govoni,CDA, RDH, MBA says. “They serve as your delivery system in the treatment room. You open your cassette, set it on the bracket tray or on the support area for the assistant, and then, when you're finished, you put the instruments in the cassette and then they go right into the ultrasonic or the instrument washer to be cleaned. Once we know that they're clean and dry, cassettes are packaged (pouches or wraps) and sterilized. So, you're handling fewer things.”
The time that cassettes save may just be a few minutes with each patient, but those minutes add up.
“Based on market survey results done by the HuFriedyGroup, it saves an average about 10 minutes per patient visit from having to handle those instruments,” Govoni says.
“It's an expense that some practices are not committed to until they see the value of extending the life of their instruments and reducing the chance employee accidents,” infection control consultant and speaker Leslie Canham, CDA, RDA, adds.
Ultimately, the organization that cassettes provide allows practices to optimize their processes.
“Everything goes back in the same cassette, and by using a system of color-coding, the instruments are placed in the cassette in a specific order,” Canham says. “Staging the instruments in the order of use makes it more efficient for the clinician to reach for the instruments. Then, after treatment is complete, the instruments are placed back in the same cassette in the same order. That can save time as well, not only from a cleaning process, but the delivery of care while using those instruments.”
Tubs
The French have a culinary phrase called “mise en place”, meaning, “everything in its place.” This phrase means having all of one’s ingredients ready before the chef starts cooking. That same concept is advised in the dental practice.
“It's a great idea to have a tub with a plastic see-through lid that has all of the materials you're going to use, that you bring into the room, rather than relying on what's in the drawers,” Canham says. “A tub can be stocked with restorative materials or endo materials or other materials that are needed. You stock the tubs with the materials you use frequently — like medicaments and materials dispensed from a multi-dose syringe. Everything in the tub is easily seen, unlike a treatment room drawer where items can sometimes roll into the back of a drawer. If you think you don’t have the dental material you need because it is unseen, you will open a new one. Later you find the old material in your drawer, but now it’s expired. So, you’re not only setting up your instruments, but if you set up tubs with your materials, it may save you money; be more efficient than having items in the room; and saves you time, because you don't have to go back and forth so much for missing items.”
Barriers
A good way to maximize efficiency in treatment room turn-around is to use impervious barriers on some equipment and surfaces. By covering difficult-to-clean surfaces with barriers, there is no need to clean or disinfect, unless the barrier becomes torn or damaged.
“I also encourage practices to take a good look at what surfaces or what pieces of equipment would benefit from barrier protection,” Govoni says. “Because if you have an impervious barrier, something like a plastic barrier, and if it's not torn at the end of treatment, you simply need to replace it. You don't need to disinfect that surface, but you have to be careful how you remove it, and you need to make sure it's not torn. That saves wear and tear on some of the equipment, and it saves a lot of time when you have to clean and disinfect the treatment room. It is also important to note that barriers used on equipment used intraorally, such as on digital sensors, must be FDA-cleared.”
Some practices may be making their workflow less efficient by disinfecting underneath the barriers or by reusing them, rather than simply throwing them away.
“One of the problems I come across is that people think they can disinfect the barriers,” Canham says. “Don't disinfect barriers. You replace them. Barriers need to be replaced after every patient.”
The impetus to do such a thing is because throwing the barrier away seems wasteful and may have a negative impact on the environment.
“Some people are concerned because of the environment; how much plastic are we sending to the landfill?” Govoni asks. “But on the other hand, if you're not using barriers, then you're using more chemicals. So, I'm not sure which is worse. And there have been some individuals that have promoted the use of reusable cloth barriers, but cloth barriers are not impervious. They really aren't going to be an efficiency tool because you're still going to have to then remove the cloth barrier and disinfect underneath it. And then you've got the issue of doing laundry. So, how many resources are we now using to launder the cloth barriers?”
Replacing the sticky barrier tape seems straightforward, but that process can also be more efficient. Often, a self-adhesive barrier will stick to itself. Canham likens it to a roll of adhesive tape.
“Think of how adhesive tape sticks to itself. It's almost impossible to find the edge,” she says. “When you place these barriers initially, instead of sticking the barrier to itself, fold the edges of the barrier to itself, so it has a little handle on each side, and it can easily be removed.”
Workflow
Once patient procedures are completed and the treatment room is to be turned around, Canham’s recommended workflow is this:
“Keep a pair of utility gloves in your treatment room, and at the end of the patient's visit, before starting your room breakdown, don those utility gloves,” Canham says. “You can start the treatment room turnaround process, place your instruments into cassettes or transport tubs or on a treatment tray. And now remove all your plastic barriers and dispose of along with your other trash.
“Still wearing your utility gloves, transport your instruments to the sterilization room, using a leak-proof tray or transport tub. Return to the treatment room, wearing your utility gloves, and start the cleaning and disinfection process,” she continues. “I like disinfectants that have both a cleaner and disinfectant in the same container, rather than using 2 different products. I also like disinfectants that are fast — 1 to 2 minutes of surface contact time. In addition, I always make sure that the disinfectant is compatible with the surfaces of my equipment. After you've completed the disinfection of your treatment room, and while you are allowing surface contact time, still wearing your utility gloves, return to the sterilization room to load your instruments and or cassettes into the ultrasonic or instrument washer, then clean and disinfect your transport tub. Before returning to the treatment room to set up for the next patient — while wearing utility gloves — disinfect them with a surface disinfectant or wash them with soap and water; then either towel dry them or remove them and allow them to air dry. While it is not necessary to sterilize utility gloves, if they are heat resistant they could be placed in an autoclave bag; and put into the sterilizer. With sterilized utility gloves, there is no need to worry about somebody else's hands being in those gloves, and it resolves the concern about utility gloves that have not been decontaminated being put back into the treatment room.”
Gloves
Hand protection and utility gloves, in particular, are an important consideration, but often misunderstood.
“Do not use dishwashing gloves,” Canham says. “They're too wimpy to protect hands from punctures. On the other extreme, don't buy bulky rubber industrial gloves. I suggest that dental teams ask their dental dealer what brand of utility gloves the other dental clients are most frequently ordering. That's a pretty good clue that that's a favorite amongst dentistry. I also recommend ordering utility gloves that can be sterilized and in multiple sizes so that coworkers and team members can find the best fit. That will address the bulky problem.”
While Canham’s recommendation is to sterilize utility gloves, Govoni offers an easier way to reprocess those gloves — but either method is acceptable.
“I may have them have their own pair in the sterilization area,” Govoni says. “Then when they're finished, they simply take a disinfectant wipe, or they can wash the gloves first, or they can take a disinfectant wipe and they wipe the gloves and then put them in a place like underneath the sink or on a hook where they can be stored until they're used again.”
Technically, those gloves don’t need to be sterilized. However, they do need to be cleaned and disinfected.
“Certainly, the ideal would be to sterilize them, but we're not even using sterile gloves for most procedures,” Govoni observes. “It is an objection that I hear from a lot of team members: ‘Ew… They're contaminated. What am I going to do?’ You simply wash and disinfect them after you use them. But keep in mind that you only touch or should only be touching contaminated surfaces with those utility gloves.”
“I tell people it's like my toilet bowl brush,” Canham adds. “It's contaminated, but I'm only ever going to use it in my toilet. I'm not going to use anywhere else. So, you're only using utility gloves on contaminated items.”
Efficiencies exist in both the sterilization area and treatment room, but they require some planning and foresight. Dental practices can optimize the workflows without sacrificing staff and patient safety.