Dental Aerosol Lessons from Emerging Research
Take a look at some of the research on ways to prevent the airborne spread of the COVID-19.
stock.adobe.com / Vectorman2017
I haven’t always been a nerd but I definitely have a healthy respect for scientists—especially those who are objective in their scientific studies.
My fascination with scientific inquiry began while studying dental hygiene at Old Dominion University, where I completed a master’s degree and conducted research. Coronavirus 2019 disease (COVID-19) was recently added to my relentless passion for periodontology and evidence-based dentistry, and I work hard to follow COVID-19 science as it changes and grows. We now know a lot more about the SARS-CoV-2 virus that causes COVID-19, including its transmission, but there’s still a lot more to learn.
Throughout the COVID-19 timeline (since the winter of 2020 to present), I’ve been closely following tweets by several aerosol engineers/scientists in order to learn more. In the early days of the pandemic, transmission of SARS-CoV-2 from person to person wasn’t thought to be through the air, and early public health messages focused on hand-washing, surface disinfection, and maintaining a physical distance to break droplet and contact transmission routes. As more scientific evidence emerged, it became clear to aerosol scientists that SARS-CoV-2 can pass in tiny droplets that waft through the air and build up over time.1
The vocal group of aerosol scientists shouting for more attention to the airborne route of SARS-CoV-2 transmission is a small but mighty group who are working hard to convince the World Health Organization (WHO) to change their public messages to acknowledge airborne transmission. These scientists are also calling for preventive measures to reduce this type of aerosol risk. In July 2020, the WHO issued a scientific brief on viral transmission that acknowledges the possible implications of such a route of transmission in crowded, poorly ventilated spaces.1
According to researchers who are now arguing for more emphasis on the importance of aerosols, governments and businesses should take specific steps to reduce this potential route of transmission. Some topics being tossed around and studied for practical application are recommendations against air recirculation in buildings and overcrowding with effective levels of ventilation with air systems to filter out particles. Businesses can also use ultraviolet light to kill airborne viruses.1
Reducing SARS-CoV-2 Aerosols in a Dental Environment
Dentistry has not shied away from implementing the best infection control practices. Many dental practices complied with the new ADA and CDC guidelines for reopening in early 2020 with a plethora of measures that were overwhelming, expensive, and ever-changing as more was discovered about pandemic transmission. Protective clothing, eye, face and mask protection, surface cleaning, and extraction of aerosols during treatment are just a few of the infection control considerations and guidance prioritized to minimize harm to dental patients and personnel. Ventilation and air filtration is another key component to reduce the risk of cross-contamination and infection.
Most of the SARS-CoV-2 transmission occurs indoors. When an infected person (or team member) enters a dental practice, 40% are asymptomatic and can spread the virus to others.2 Once the virus enters the practice, there are 2 choices to keep it from infecting someone: either bring in fresh air from the outside or remove the virus from the air inside the dental practice.2 The more fresh, outside air inside a building, the better. Early on in the COVID pandemic, I read a brilliant hospital suggestion from a retired RN that stated:
Hospitals today could purchase hundreds of inexpensive breeze fans, seal them in windows, and create hundreds, even thousands, of negative pressure rooms in a day. The negative pressure will prevent viral particles from escaping from the room and exposing staff and other patients.3
According to an aerosol scientist, the exact rate of air exchange in a room depends on the number of people and the size of the room.2 Most experts consider roughly 6 air changes an hour to be suitable for a 10 x 10 ft room with 3 to 4 people in it, but exact air changes an hour during a pandemic may be higher.2
Air Purifiers
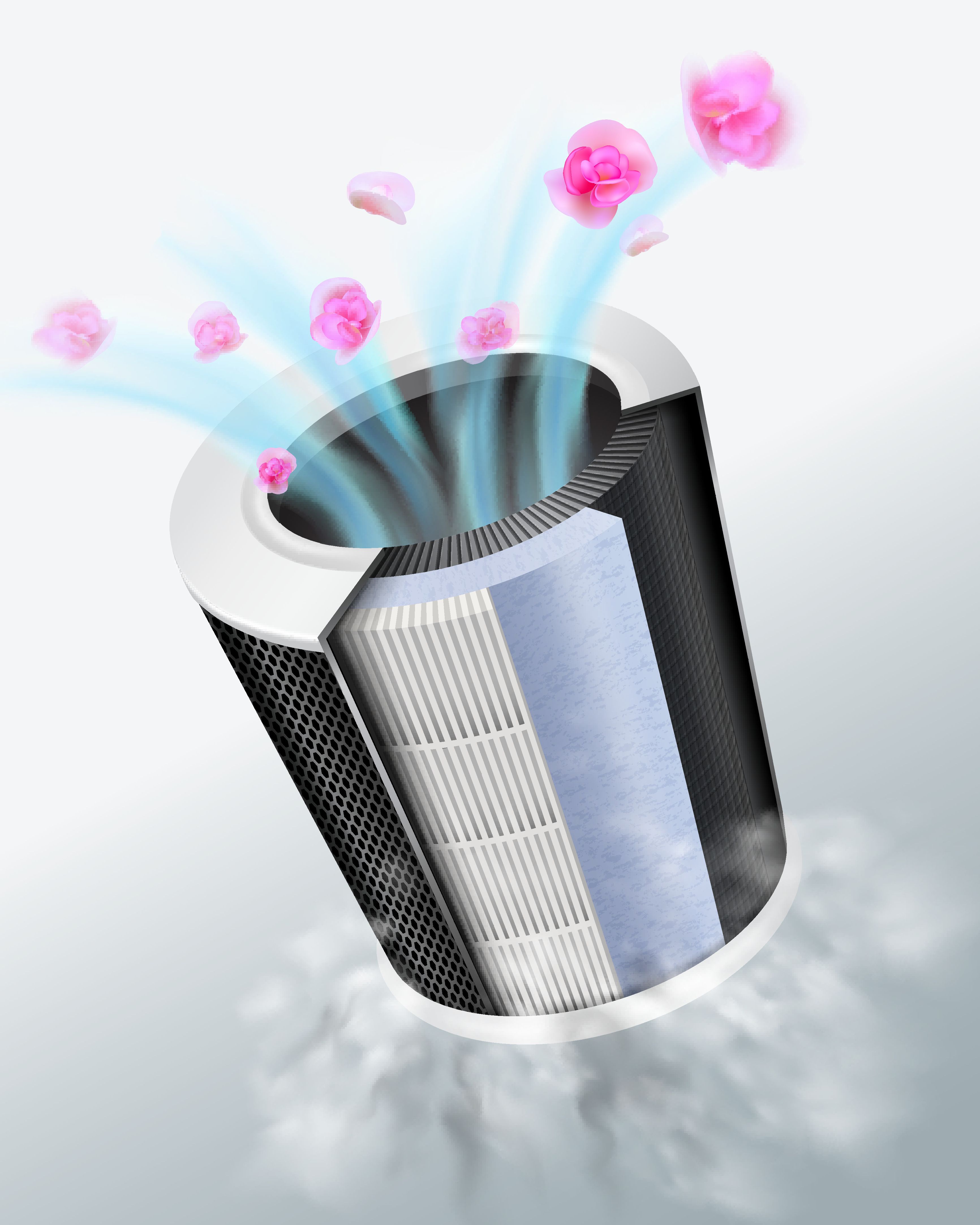
Air cleaners, commonly called air purifiers, remove particles from the air, usually using a filter made of tightly woven fibers.2 High-efficiency particulate air (HEPA) filters were invented back in the 1940s, so they are nothing new. They can capture particles containing bacteria and viruses and can help reduce disease transmission. There is a lot of misinformation about air purifiers with HEPA filters. Aerosol scientists state HEPA filters effectively remove all particle sizes of relevance, which includes SARS-CoV-2 particles. Air purifiers with HEPA filters remove 99.97% of all particle sizes.2,4 Because recent evidence demonstrates that SARS-CoV-2 can remain airborne longer and travel farther than anticipated earlier in the COVID-19 pandemic, HEPA filters have been recommended.5 The CDC states that dental offices should consider air purifiers with HEPA filter mechanisms as an adjunctive means for decontamination of SARS-CoV-2 while the patient is undergoing, and immediately following, an aerosol-generating procedure. They also recommend selecting a HEPA air filtration unit based on the Clean Air Delivery Rate (CADR).6
Far-UVC Light
Another new approach that limits transmission emerged from research conducted at Columbia University and may eventually become a major public measure.7 Far-UVC light kills pathogens, including SARS-CoV-2 and is a germicidal UV light without health hazards to skin and eyes (207-222 nm compared to 254 nm germicidal ultraviolet light that causes damage to human tissues.)7 According to the Columbia University research team, continuous far-UVC exposure in occupied public locations would result in approximately 90% viral inactivation in approximately 8 minutes, 95% in approximately 11 minutes, 99% in approximately 16 minutes, and 99.9% inactivation in approximately 25 minutes.7 Applications for the dental office could include continuous low-dose UVC exposure lamps (if reasonably priced like LED light bulbs) that could help reduce the probability of person-to-person transmission of COVID-19, as well as other seasonal viruses like influenza.7 As patients look up at the ceiling from their dental chair, an overhead, flush-mounted light just might be a far-UVC exposure lamp instead.
With research continuing on the SARS-CoV-2 virus, best practice recommendations are likely to keep changing. We now know a lot more about the virus and the disease it causes than we did when the dental industry shut down in March, and as additional information is revealed by research, new ways to protect ourselves and our patients will emerge. Paying attention to the emerging science around the pandemic is important as it keeps us up to date on all of these new precautions, best practices, and technologies.
References:
- Lewis D. Mounting evidence suggests coronavirus is airborne — but health advice has not caught up. Nature. 2020;583(7817):510-513. doi:10.1038/d41586-020-02058-1
- Miller S. How to use ventilation and air filtration to prevent the spread of coronavirus indoors” The Conversation. Published August 10, 2020. Accessed September 18, 2020. https://theconversation.com/how-to-use-ventilation-and-air-filtration-to-prevent-the-spread-of-coronavirus-indoors-143732
- Retired RN says OTC window fans could create negative pressure rooms fast. Phillylabor.com. Accessed September 18, 2020. http://phillylabor.com/retired-rn-says-otc-window-fans-create-negative-pressure-rooms-fast
- Zhao B, Lie Y, Chen C. Air purifiers: a supplementary measure to remove airborne SArs-CoV-2. Build Environ. 2020;177:106918. doi:10.1016/j.buildenv.2020.106918
- Nazarenko Y. Air filtration and SARS-CoV-2. Epidemiol Health. 2020;42:e2020049. doi:10.4178/epih.e2020049
- Coronavirus disease 2019 (COVID-19); Guidance for dental setting. Centers for Disease Control and Prevention. Updated August 28, 2020. Accessed September 18, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
- Buonanno M, Welch D., Shuryak I, Brenner DJ. Far-UVC light (222 nm) efficiently and safely inactivates airborne human coronaviruses. Sci Rep. 2020;10(1);10258. doi:10.1038/s41598-020-67211-2
