Top tips for handpiece infection control
Ensuring that these devices are properly maintained is critical for their longevity.
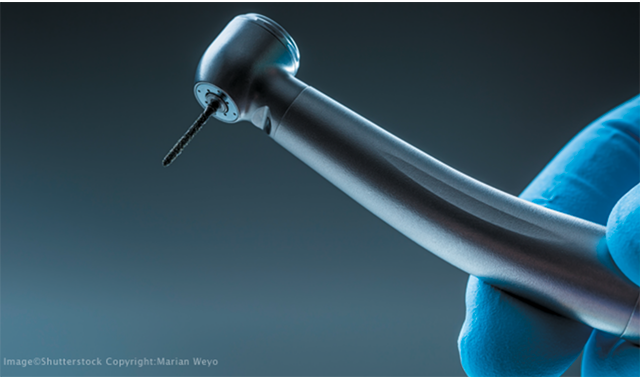
Probably the most ubiquitous piece of equipment in the dental practice is the humble handpiece. It isn’t just there to strike fear into the hearts of patients; it’s the workhorse of the practice. Unlike some other instruments and pieces of equipment requiring upkeep, handpieces are delicate, precision-engineered devices that demand their own unique care.
Manufacturer’s instructions
“The office needs to make sure they get the instructions for use with the new device,” says Peggy Spitzer, a dental hygienist and clinical education manager for Certol International. “A lot of times, it’s Christmas morning and they’re ripping open the packaging and excited to use the device, but they have to make sure that the instructions are not discarded.”
But, before that device even gets placed into service, it must be understood.
“Someone will have the not-pleasant task of going through the instructions and finding things in there that may be confusing or perhaps just flat-out wrong,” she continues. “And that takes some knowledge on the part of the person that’s reading instructions to even figure out, ‘This doesn’t sound right.’”
While that chore may sound time-consuming and overwhelming, Spitzer points out that it would be easier on staff if manufacturers did more to reconcile their instructions for use (IFU).
Related reading: Should you be concerned about measles?
“I think where it really is pretty harsh on the dental staff is to tell them, ‘You’ve got to follow the instructions,’ and then turn around and say, ‘Well, some of it is wrong. You figure it out and then call us,’” she says. “The one I’m most aware of is that handpiece manufacturers will tell the users to clean the handpiece with alcohol. That is the No. 1 defect from an infection control standpoint. They tell these folks to clean the handpiece with alcohol, and that is a failure because isopropyl alcohol is not a cleaner.
“It’s not even a validated disinfectant because it doesn’t have an EPA registration. It actually causes blood to stick more,” she continues. “So, instead of cleaning off the blood, it’s actually causing the blood to do what we call ‘denaturing.’ It’s kind of like what happens with eggs when they’re cooked and allowed to dry. The alcohol denatures the protein and makes it stick harder. This may happen because instructions are written by engineers and not infection control experts. If instructions for cleaning are confusing or could create problems, call the handpiece manufacturer for written clarification.”
Best practices
While each handpiece model will have its own IFUs, there are general cleaning and maintenance steps that hold true for all handpieces. Regrettably, those steps are often misunderstood.
“The biggest problem is they’ve never really been properly educated on the process with what happens from that handpiece from the time it is done with a procedure in the operatory until the time that it is put into the sterilizer,” says Eric Ozelski, North American product manager, SciCan. “There’s a bunch of sequential things that should happen. A lot of that can be due to the fact that they’re not reading the IFU. If you look at a number of manufacturers, almost all of them follow the exact same protocol from the time that it leaves the operatory until the time that is put into the sterilizer.”
The first step, he says, is cleaning off the handpiece. But, even that first, seemingly simple step is often performed incorrectly.
“We did some surveys a number of years ago, from 2012 to 2016, about this step in the process, and about 65 to 70 percent of dental offices are using a disinfectant wipe to externally clean the handpiece,” Ozelski says. “If you go into a steak restaurant and you’re sitting down for dinner, but you’re afraid that the knife isn’t clean, would you take out a chemical-based disinfectant to clean off your fork and knife and then start to eat your food? No.
“And why is that?” he continues. “Well, there will be chemicals left on there. So, why is it okay when you have a handpiece that’s going to be touching mucus membranes and part of this process of cutting teeth, why would we use that chemical on that? Most manufacturers’ protocols will tell you to use some running water and a soft bristle brush to clean off the exterior of the handpiece. What we’re really looking to do is clean the exterior of debris. We’re not looking to disinfect it because we still have to go through the sterilization cycle.”
More from the author: The top 10 best cities for dentists in 2019
Once that step is completed, the handpiece should be safely transported to the sterilization center. Ozelski notes that the handpiece-as well as all other dental instruments-should be transferred to the sterilizer in a covered, sealed container. After the cleaning process, the handpiece should be lubricated and then purged.
“If we’re in a sterilization area that doesn’t have an automated device, like the SciCan STATMATIC, that staff member then has to walk back to the operatory to purge that handpiece for up to 20 seconds,” Ozelski says. “From some of the surveys that we did, about 65 percent of staff members would lubricate the handpiece but not purge it, and they would immediately put that handpiece into the dental sterilizer. The problem with this is if we’re not purging out that excess oil and the debris, all of that stuff is still located inside of the handpiece, and then we’re bagging that handpiece with a bunch of junk still in it and we’re baking it into the working components of the dental handpiece during the sterilization cycle.”
The result of that improper maintenance can be a very unpleasant, very visible presentation.
“Often, there will be staff members who complain, ‘My bags are turning brown with my handpieces,’” Ozelski says. “That’s the case because you’ve introduced this lubricant and there’s still dirt in the handpiece. Now, all of a sudden, you’re heating it up and brown ooze is coming out of the handpiece and some of that oil and debris has been baking onto the components of the handpiece.”
Continue reading on page two...
Have enough on hand
Ozelski observes that many practices don’t have enough handpieces to do the job properly. The magic number? Three per operatory.
“One would be in use, and one would be going through the maintenance cycle,” Ozelski says. “The goal would be to have the third one already sterilized and ready to go for the next patient. Or, if for some reason the handpiece to be used becomes compromised, it becomes the backup.”
However, with three handpieces for each operatory, costs can add up quickly.
“There’s a reason why a lot of dental handpieces, especially premium handpieces, cost anywhere between $1,300 and $1,600,” Ozelski says. “It’s because they’re workhorses. They’re made to tolerances that aren’t seen in a lot of industries out there. And they’re what generate the money for the dentist.”
For example, if the practice has five operatories and only one handpiece in each, bringing on additional equipment can be costly.
Trending article: 10 questions to test your understanding of infection control requirements
“All of a sudden it’s like, ‘Oh, well, you’re telling me I need two more per operatory. You’re asking me to spend an additional $15,000.’ But, you’ve got to look at it this way: We’re trying to protect our investment and to prevent downtime waiting for a handpiece to be sterilized. The best way to do that is to have three in rotation. You’re going to get a lot more longevity out of the handpiece by maintaining it properly.”
Do your research
Because handpieces are expensive and delicate pieces of equipment, it’s wise to spend some time researching before a purchase is made. And that research doesn’t just include cost or operating parameters; it’s also a good idea to dig a little deeper and look over the instruction manual.
"When they’re making an investment in a device and it’s something that’s going to go inside the patient’s mouth, they should be reading or obtaining the instructions or finding more about how to maintain and reprocess the device from the manufacturer,” Spitzer says. “That pushes the manufacturers to give them all this information before they make a decision to make a purchase.”
Failing to do enough research on a device is a common enough problem, but one that can be avoided.
“It happens everywhere,” Spitzer says. “It happens in big hospitals. It happens in little dental clinics. They’ll buy equipment before they research it, and then they have purchased something that’s going to be very difficult to maintain, and especially to reprocess, to use on another patient.”
Handpieces are critical pieces of equipment; devices that are necessary to perform effective dentistry. Ensuring that these devices are properly maintained is critical for their longevity.
Maximizing Value: The Hidden Benefits of Preventing Hospital-Acquired Pneumonia Through Oral Hygiene
September 10th 2024Originally posted on Infection Control Today. Hospital-acquired pneumonia (HAP) is a significant infection prevention concern, leading to high patient mortality, increased health care costs, and ICU usage. Oral hygiene is an effective preventive measure.