Implanting success: The state of dental implants
Dental implants are nothing new. While they have been around in one crude form or another for thousands of years, the breakthrough that led to modern day implants didn’t occur until Per-Ingvar Brånemark’s mid-1960s work with dental osseointegration. And it wasn’t until the 1980s that implants became a widely available option.

Dental implants are nothing new. While they have been around in one crude form or another for thousands of years, the breakthrough that led to modern day implants didn't occur until Per-Ingvar Brånemark's mid-1960s work with dental osseointegration. And it wasn't until the 1980s that implants became a widely available option.
Now, however, thanks to technologies such as CAD/CAM and cone beam scans, precision-made hardware, and surgical techniques, implants can be done with positive, predictable outcomes and speedy patient recovery times.
Technological innovation
Because of technologies like CAD/CAM, crafting the implant is much easier, faster and of consistent quality.
"Labs have gone wholeheartedly toward CAD/CAM in every way-designing frameworks, even provisionals, and more," says Dr. Allan Pollack, DDS, president of the Academy of Osseointegration. "And more doctors are incorporating it into their practices as well, whether they have an in-house unit where they are doing their own milling, or they are using CAD/CAM technology to design restorations."
Dr. Neal Patel, DDS, of Infinite Smiles in Powell, Ohio is one such clinician who has embraced technology for improved implant cases.
"The new philosophy that we've all pretty much adopted is restoratively driven implant planning and the concept of the guided surgery for accuracy, and then the use of CAD/CAM technology for precision in the fabrication of the prosthetics," Dr. Patel says. "That process starts with having the ability to design a restoration, virtually, using digital technology like CAD/CAM. That virtual tooth is something that can happen in two locations: There are labs that can do it routinely, but there are some doctors who actually have CAD/CAM in the office, and that's our scenario here."
Dr. Patel is somewhat unique in that he has an in-house lab technician who manufactures most of his cases.
"When a patient comes in and they're missing a tooth or multiple teeth, we can actually take a digital intraoral scan and I can either send that to my [dental technician], Marina, and she can virtually design the teeth in software that's perfectly matched to the patient's esthetics and send that virtual plan back to my office," Dr. Patel says. "Or if I have time, I can do that process myself. We have a virtual wax-up done in the CAD/CAM software."
Manufacturing implants chairside is not right for every case, but when it can be done, it's a welcome solution for both doctor and patient.
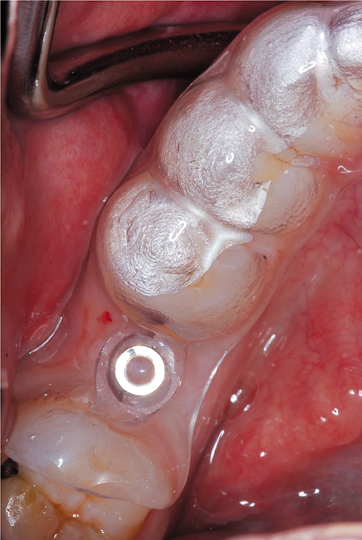
"It's pretty awesome," says Dr. Kaveh Ghaboussi, DDS, of Madison Smile Solutions in Madison, Wisc. "You can't do it all the time. There are situations where it's better to either scan the implant or take an impression and have the lab do it, but a lot of times when the implant is ready to restore, we can take a stock abutment, and we can scan it in the patient's mouth and mill a crown right there, which is pretty great. And we have even placed an implant and milled a crown and put it on all in one appointment, which is a pretty advanced thing to do. It cuts out a lot of time and a lot of visits for the patient when you can do it."
Overall, technological advances have dramatically improved the quality of care patients receive.
"All of this technology can speed up treatment times while also resulting in higher-quality outcomes," says Dr. Robert Gottlander, VP, Global Prosthetic Solutions at Henry Schein. "You can take digital impressions with an intraoral scanner, design the position of the teeth, and then take that design file from the cone beam and to do the implant planning. There are so many things that you can do today that you could not do five or 10 years ago. And while the technology itself is very impressive, it's what the technology can do for your patients and your practice that enhances its value. And besides saving time and increasing accuracy, an integrated digital solution that includes plan management software, such as Dentrix, can make insurance reporting and reimbursement easier, increase profit per patient, and lead to a steady flow of new patients either through referrals or by using social media to advertise the convenience of digital dentistry."
Patient awareness
New technologies and workflows allow patients to have a better understanding of their dental needs, and this is especially the case where implants are concerned.
"It all starts with diagnosis," says Dr. Gary Severance, DDS, Planmeca University. "It improves not only the patient awareness, because patients don't go to a dentist and say, ‘I need an implant.' They present with an edentulous space or a missing tooth, and they want to know what options are available to them. Typically it may take several appointments before the patient can hear the optimal treatment alternatives. The dentist may make impressions, get study models then have the patient back to discuss viable options, whether it's an implant solution, orthodontics or fixed prosthodontics. With CAD/CAM dentistry in the office, there is no waiting to show the patient their situation-simply scan and you will have your virtual model to display. Patients see their personal situation rather than using display or instructional models. It's personal and they buy-in to the evident issues and solutions.
"After being shown their condition, the dentist can then use CAD/CAM tools and smile design software to help develop a treatment plan. When combined with other 3D technologies like cone beam, now you can plan the implant therapy completely out and discuss visually with the patient their individual situation."
Pilot drill use on guide. Note the stop on the pilot drill.

Eliminating surprises with cone beam scans
Like many dentists performing implants, Dr. Ghaboussi starts with a cone beam computed tomography (CBCT) scan. Cone beam scans give very detailed representations of the head, showing bone and tissue in unprecedented detail.
"That scan is a pretty important part of the workflow, because it tells us what the complications will be, if any, and the risk to the patient. Do we want to do it? Do we not want to do it? It eliminates surprises," he says. "Once we have the scan, it's pretty easy planning the case."
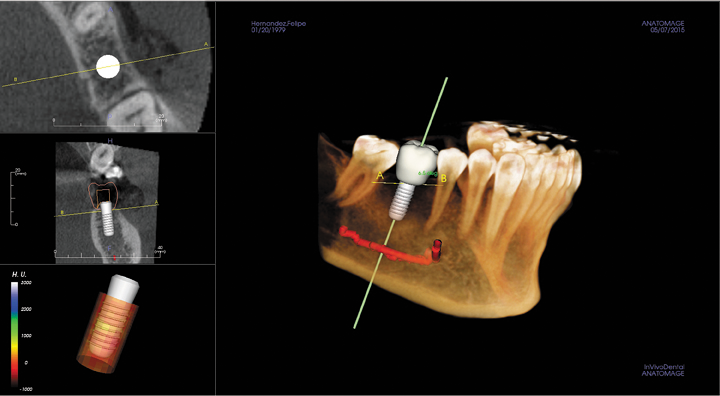
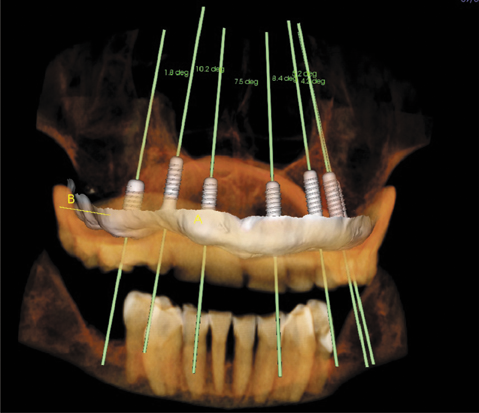
Once the scan is taken, the case is designed in specialized software.
"We use CLINIVIEW in Anatomage," says Dr. Ghaboussi. "There's a lot of software out there, but they're so user-friendly and easy to use. The CTs are super accurate, so we can plan a case by doing what I call a ‘virtual surgery,' which is where we can look in 3D at the bone structure and tissue and place the implant on the computer before we do anything to the patient. We know exactly what we have to do, exactly where we have to put an implant. We know pretty detailed information so that we can predict any kind of problem that might arise and have a contingency plan for it before we even start. Doing all that is not only good for the patient-because no patient wants complications if they can help it-but it makes it a lot more efficient, because the surgical times are a lot shorter. We can do more work in 15 minutes than maybe I could have done in an hour, previously, and who wants to be under the knife for an hour when they could be under the knife for just 15 minutes?"
Surgical guides
When it comes time to perform the implant, doctors can turn to surgical guides to ensure they are drilling in the exact location with the precise angle and depth. These guides are made, most often, by the lab, but sometimes can be fabricated chairside, based on the scan data.
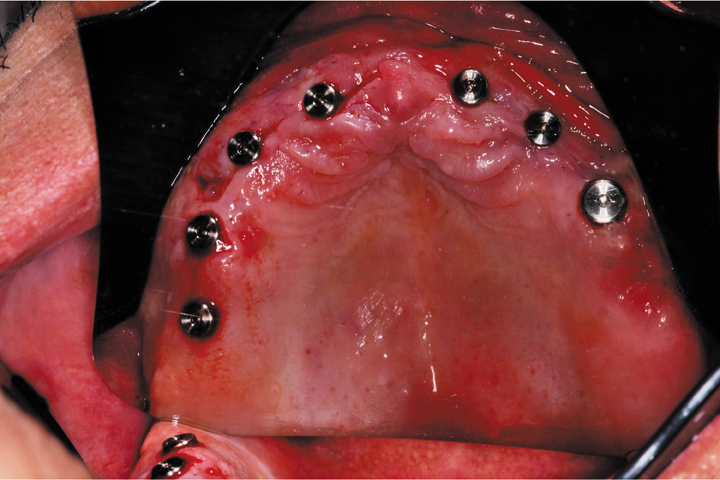
Virtual surgery with virtual restoration
"If the case is ideal and just seems super easy, I will freehand it," Dr. Ghaboussi says. "But if there is any kind of tricky part to it or angulation or the access is difficult, we just go ahead and have a surgical guide made. The cost of a surgical guide has come down significantly, so it just makes the workflow so much easier and cuts down on wasted time. The surgical guides can really simplify the case. Even if you're removing 20 teeth and leveling bone and placing implants, for me that would have been a half-day procedure-start at 7 a.m. and finish at 1 p.m. And now you can do that in an hour or two, using surgical guides. The labs make a bone-leveling guide, so you extract the teeth and flap back the tissue, and the lab has made a guide that you put over the bone. Then you just flap-out down to the level of the bone, and then you place the implant guide on the bone and screw it in so it can't move, and then you place the implants and you're done."
Surgical guides are not new creations, but advances in manufacturing have made them less costly and more readily accessible to doctors.
"In the past, surgical guides were not used very often because they were difficult to make and they were costly to make," Dr. Patel says. "It was a very cumbersome process to order surgical guides. There are newer technologies that allow clinicians to make them in as little as 40 minutes, chairside, while the patient is waiting using milling technology. With digital communication and software, the labs can also receive digital files, and once they receive the digital file the workflow is accelerated where they can quickly design the surgical guide and produce it with very little effort using 3D technologies. It's not an absolute thing where all clinicians have to use them, but we hope, collectively, that someday it will be the standard of care to use surgical guides, because there's really no argument against them other than cost."
Better predictability, outcomes
As with any other dental innovation, implants continue to get better and better-not only from the technology, itself, but also how patients respond to them.
Demonstration of the use of Pilot drill with a built-in stop with the semi-guided technique.

"I've been doing implant surgery since 1986 when Brånemark first came out," Dr. Pollack says. "It's dramatically different since then, certainly. The surgeries are much simpler. We used to use full-sterile techniques. That's gone. Healing times are shortened dramatically. It used to be six months on the maxilla, now it's two or three, depending on the circumstances. In most cases it's six weeks for a number of implants, and then for one or two of them on the market it's as little as three weeks healing time in native bone. They're easier, quicker. The success rates have improved as well. The success rates are in the mid to high 90s across the board now."
And because of the improved outcomes and simplified procedures, patients are happily surprised.
"Patients come into the procedure anxious and nervous, the first thing that nine out of 10 patients say is, ‘Wow,' " Dr. Patel says. "The second thing many say is, ‘Is that it?' And then we get a little hesitant, because implants are still costly, and we sometimes worry that we're charging too much for such a little amount of chair time. Today, with minimally invasive surgery, because everything is designed using a 3D X-ray, we can avoid a lot of the large invasive flap designs and some of the large exposures to the bone, because we have the ability to see the bone in the software and don't necessarily need to make a large incision. So we can be conservative in the approach, and that allows the patient to have a better experience both during surgery and certainly afterwards."
Design
Implant design has improved over the years, offering new features and affording better esthetics, precision and quality.
"Over the course of the past 20 to 30 years of implants being placed routinely, we learned a lot of important features from a design standpoint that implants should have in order to maintain their lifespan," Dr. Patel observes. "There are a lot of engineering design features including different sizes of threads and different thread patterns, in addition to different sizes of implants so they can be more customized to the patient's anatomy. Most importantly, they have newer surface technologies, so the implants, themselves, are usually pure titanium or titanium alloy. Once they are machined, they're further treated in a lab environment where there are surfaces that are either roughened and chemically treated surfaces that are better from a biocompatibility standpoint. That also accelerates the healing process."
Not every new feature is revolutionary, and it is important to really understand implant qualities before deciding which one to use.
"Implant design is always evolving, and some of it is important changes to implant design and other things are not so important," Dr. Ghaboussi adds. "There are many studies that implant companies put out that say their design is better, but when you look at unbiased research, the success rates are very similar across the board. You haven't really seen the changes in the past few years. When they started out 30 years ago or so, there have been a lot of changes since then that make the implants more stable, less likely to lose bone around them. But in the most recent years, the changes to implants have not been really drastic changes. If you're placing a titanium implant, chances are you are going to be fine as long as it's from a reputable source. The CT will help you do it in the best way possible that would give the best chance for long-term success."
Esthetics
Esthetics is one area where improvements continue to evolve, thanks to improvements in materials, engineering, CAD/CAM and hard work and collaboration between the doctor and the dental lab.
"That's an area where there's been a lot of change in the last few years, because now people are milling restorations in their offices," Dr. Ghaboussi says. "They're making restorations right there at the same appointment, and that's been a huge change, because it wasn't as common in previous years. So if a dentist is using a lab, then it's really incumbent on the dentist to communicate what they want with the lab. There should never just be a one-way street where you send something to the lab and they send it back to you and you have no input into what you get back."
Virtual surgery provides confidence during the surgical phase.
Improved designs have also resulted in better quality esthetics.
"We're getting phenomenal results because there are newer concepts in the restorative process for implants," Dr. Patel notes. "There's a new process called TiBases. The TiBase is very low in profile and subgingival, so we can really customize the emergence of the restoration from the gum tissue. There is a lot of ceramic material, as opposed to titanium, which allows us to then have a more predictable esthetic result near the gum line and certainly the top of the tooth itself. The ceramics are now at the point where we can mimic existing teeth, regardless of their characteristics and color. They've come so far, I would say we are close to the edge of where we're getting perfect results, esthetically, where they're not detectable by the untrained eye."
And the doctor's technique has also enhanced overall esthetics.
"Esthetics are dependent on appropriate placements and tissue management," Dr. Pollack says. "While on the one hand surgeries have gotten more predictable and easier, there are still potential pitfalls if you don't pay attention to basic principles. You can accomplish great esthetics with implants, if you manage the tissues properly, both hard and soft, and don't place an implant in an improper position; it still comes down to that. You have to place the implants in the ideal position and you may need to manipulate the hard and soft tissues so that you can do so."
Work together
It is incumbent on doctors and their laboratories to communicate and collaborate on their cases. Happily, digital dentistry has made that collaboration much easier and more effective.
"Successful laboratories have very often been successful, because they have a close collaboration with the dentist," Dr. Gottlander says. "In many situations, laboratories have supported the dentist with knowledge, and I think that will continue. What the technology is doing is that you can actually communicate much faster and more directly between the dentist and laboratory. Let's say if I do a scan and I send it to my lab to design an abutment, the lab can send that design back to me so I can check it on my screen in my office. I can approve it or ask for [a] change. I also think that communication between the dentist and the laboratories, when it comes to implants, is OK, but it [can] be taken farther with new technology, that's for sure."
Collaboration can sometimes depend on the equipment the doctor and lab have, so it is important to know each other's capabilities. Labs tend to be farther along the curve when it comes to technology adoption, so it is a good idea for the doctor to seek the lab's advice when considering major purchases.
Immediate post-surgical photo
"I know some hesitate to purchase technology thinking that it will soon be outdated or may not provide the claimed benefits. The last thing offices need is a technology that sits in a corner and is not adding to their practice evolution, or technology that's closed and not compatible with future investments," Dr. Severance notes. "Before an office invests in new technology, they should essentially treatment plan their office. It might be a staged incorporation of technology-this year chairside CAD/CAM, next year cone beam, or centralizing patient management systems. Manufacturer and distributor representatives as well as peers can be a vital source of guidance. If you look long-term and comprehensively, you can really evolve the practice and provide patients and your team with better dentistry."
Making sure that the doctor's office can communicate with its lab is critical. While manufacturers are embracing the notion of open systems-that is, systems that can communicate with those made by different manufacturers-not all components can speak to each other.
"You need connectivity between the dental practice management software and the laboratory management systems," Dr. Gottlander says. "Interoperability between different digital technologies is essential. Plus that interoperability adds to the accuracy and time-management aspects of the relationship between dentists and the laboratory, reducing errors and decreasing costs."
To meet that need, Henry Schein offers its Digital Dental Exchange (DDX) service to help labs and practices communicate.
"You can use most scanners today with the DDX software and be sure that you have the same file format all the way from the scanner in the dental office to the laboratory," Dr. Gottlander explains. "What we have seen is that most of the questions asked today are not specifically about individual pieces of equipment. Most people ask about how to get different technologies to work together and to make sure that there is a predictable outcome, quality and timeline."
The future
Looking forward, Dr. Pollack expects to see similar improvements in quality and innovation that we have already seen.
"I think we're going to continue the same trends that we are in now," Dr. Pollack muses. "I wonder if we're going to get to a place where we get into custom medicine. I wonder if we're going to get to that point in implant dentistry, where you'll take a digital scan and a CAT scan of a patient, and from the digital data, before you extract the tooth, you'll have a custom 3D printed titanium implant, and you just extract the tooth and place the implant in position. I don't know if we're going to get to that point so fast, but that's kind of the direction we're heading. A lot of the work is going to be taken out of the factory or the lab and brought into the office."
This photo shows the guide in place.
While technology and techniques will certainly continue to evolve, Dr. Pollack warns that doctors should be competent to do the work and not just offer it simply because they can.
"The one thing I'm concerned about is, as the implants become more predictable and the surgeries are easier, people think that they don't need to have the same level of basic knowledge and training, because there are still complications, there are still problems," Dr. Pollack notes. "You still need to pay attention to the biology, so the weekend warriors in dentistry are not necessarily the best thing for the profession and the public. I remind people that it behooves them to apply appropriate levels of training, not just the occasional course here and there, and learn how to drill a hole. It's not quite that simple."
Dr. Gottlander notes that the current state of dental implants is even more astonishing now than when they first became widely adopted in the 1980s.
"The early days were extremely exciting. But what we have today, all of the different potential combinations of equipment and the possibilities they have opened up, has taken things to a whole new level," Dr. Gottlander says. "There has never been a time in dentistry where practitioners and patients have had so many choices."
Clinical photos courtesy of Dr. Kaveh Ghaboussi
ACTIVA BioACTIVE Bulk Flow Marks Pulpdent’s First Major Product Release in 4 Years
December 12th 2024Next-generation bulk-fill dental restorative raises the standard of care for bulk-fill procedures by providing natural remineralization support, while also overcoming current bulk-fill limitations.