How direct access is expanding treatment options for patients
With more patients requesting after-hours appointments or mobile dental care, hygienists in direct access states are making a difference.

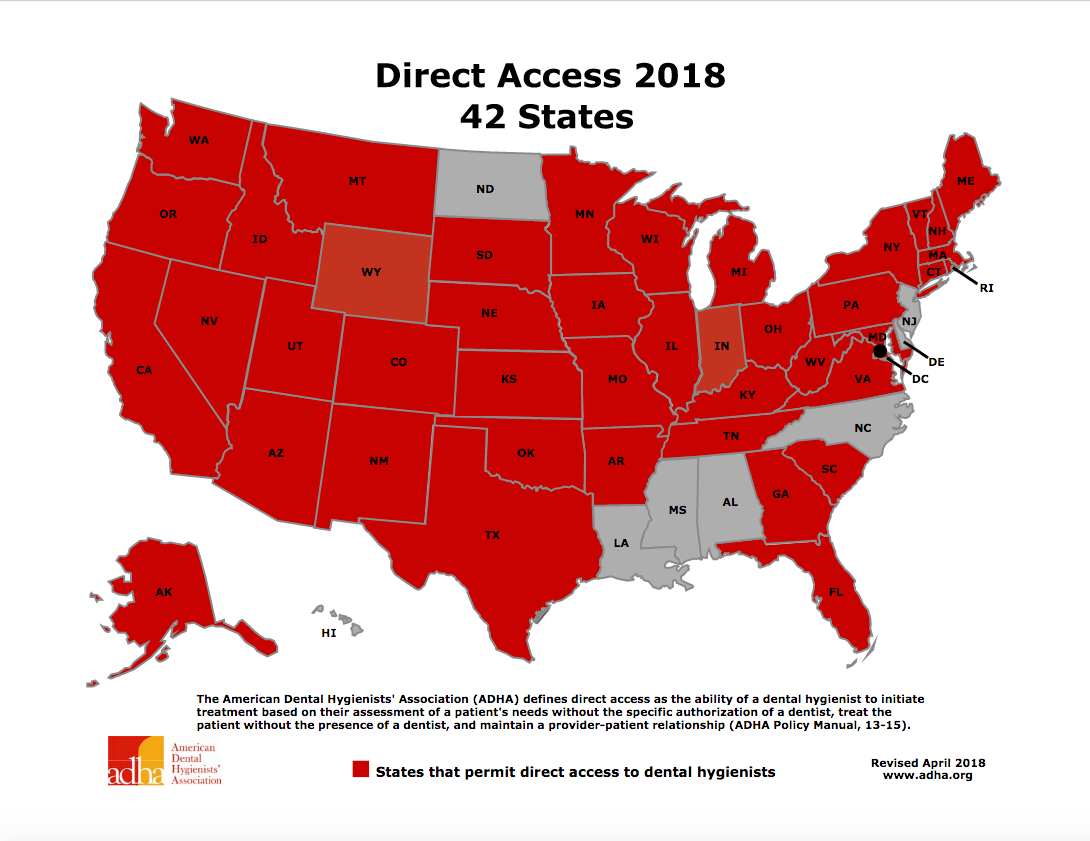
About 10 years ago, only 28 states allowed direct access. Compare that with today where 42 states allow it – and the support for direct access is continuing to grow.
The American Dental Hygienists’ Association defines direct access as “the ability of a dental hygienist to initiate treatment based on their assessment of a patient’s needs without the specific authorization of a dentist, treat the patient without the presence of a dentist and maintain a provider-patient relationship.”
“As the hygiene association, we really promote that dental hygienists are integrated into the healthcare delivery system, and so through that direct access system that provides for that,” says Ann Lynch, director of education and professional advocacy for the American Dental Hygienists’ Association.
While rules and regulations for direct access vary per state, most allow for “general supervision” duties on patients of record, according to the California Dental Association. These duties include such procedures as scaling and root planing, sealant application and oral prophylaxis, among others.
Trending article: 4 movement strategies for a pain-free dental career
Other states are trailblazers, allowing hygienists to perform a full scope of care. Take Colorado, for example, which has been allowing dental hygienists to practice without the direct supervision of a dentist since the early 1980s. According to the state practice act, hygienists can perform unsupervised procedures such as taking X-rays, doing periodontal charting and even providing dental hygiene diagnosis. Indirect supervision, which means that a dentist doesn’t need to be present but must have prior knowledge and consent of the procedure, covers things like local anesthesia, silver diamine fluoride, interim therapeutic restoration and lasers.
“Not everybody is able to come to a brick-and-mortar practice in a metropolitan area,” says Alyssa Aberle, a registered dental hygienist practicing in Colorado and executive administrator of the Colorado Dental Hygienists’ Association. “I think when hygienists are able to practice either unsupervised or under general supervision and provide direct access, you really open up the options for patients of how and where they can get care.”
What direct access means for hygienists
Hygienists who are interested in performing general supervision duties must be aware of specific continuing education requirements, which vary from state to state. In Colorado, for instance, hygienists must perform 30 hours of continuing education every two years. Some procedures, such as local anesthesia and silver diamine fluoride, require their own separate permit, Aberle says.
In other states, like Oregon, hygienists can obtain an expanded practice permit and enter into a collaborative agreement with a dentist to provide such services as administering local anesthesia, administering temporary restorations without excavation, and prescribing prophylactic antibiotics and nonsteroidal anti-inflammatory drugs.
“Clinicians who desire this additional responsibility have a few requirements,” says Tina Clarke, a registered dental hygienist practicing in Oregon and a previous president of the Oregon Dental Hygienists’ Association. “They must provide documentation for a certain number of hours (about 2,500) of patient care and have very specific continuing education courses. In Oregon, the normal CE requirements are 24 hours every two years. For EPP hygienists, they need to have 40 hours every two years. EPPs must also carry professional liability insurance as well as have a current BLS (basic life support) for the healthcare provider card.”
For hygienists looking to be their own boss, Colorado allows dental hygienist to open up their own dental hygiene practice, which can be either a mobile clinic or a brick-and-mortar office.
Aberle says allowing hygienists to practice unsupervised is especially helpful for school-based settings and rural areas.

“Colorado is one of the states where we definitely don’t have a shortage of dentists. We have an abundance of dentists, but they’re all in the metro areas. So we have the other three-quarters of the state that’s rural and no dentists are moving there, but there are hygienists who live there and are willing to provide care. That really opens up options for them,” she says.
Another path to provide direct access is through dental therapists. In 2009, Minnesota became the first state government to authorize the licensing of dental therapists and required that these providers primarily serve underserved patients. Other states such as Alaska, Maine and Vermont have since followed suit.
More from the author: Can opioids prescribed for wisdom tooth extraction lead to long-term drug use?
“Dental therapy is another way that dental hygienists can take their education and experience and provide further services with additional education,” Lynch says.
In terms of providing greater access to care, dental therapy seems to be making a difference. Lynch notes a study done by the Minnesota state department and the Minnesota Board of Dentistry that showed the total number of new patients served by dental therapists at study clinics over an almost two-year period was 6,338.
“I think it’s reasonable to correlate that many of those patients perhaps would not have received care without having the dental therapists as a part of that team,” Lynch says.
Up next: What direct access means for patients...
What direct access means for patients
The cost of healthcare continues to be a hot topic in the country. The cost of dental care is one of the reasons Aberle says dental hygiene offices are doing well in Colorado, especially those in rural parts of the state.
“Some of the patients that they see just don’t have a lot of dental needs; they really just need preventive care,” she says. “So why go to the dentist if you don’t need restorative work? It might be faster, easier and cheaper to just see a hygienist.
“To me, the idea of our economy is people have choices and they have choices of when and how they can get their care. Sometimes that’s a more affordable cost, especially if you have a mobile practice because you don’t have as much overhead, so sometimes you can offer the services at a more affordable price for certain populations.”
Read more: 5 ways for hygienists to deal with parents of patients
Hygienists also serve an important function for the elderly. As the Baby Boomer generation continues to age, many are finding it difficult to travel to a physical dental office. Having hygienists visit nursing homes or set up mobile clinics in the community - or even visit a patient’s house - can be a game-changer.
“Some of our patients who aren’t elderly but still have either mobility issues or transportation issues, they’re not able to travel an hour to go to a dental clinic,” Aberle says. “So if you have hygienists who can come to them or closer to them, then that definitely helps.”
Clarke says she’s had the opportunity to provide care without a dentist being present in the office, and she’s seen the benefits first-hand.
“Patients were extremely happy they could still continue on with care while the doctor was out. If needed, I could also provide triage care for the patient until the doctor could be in either later in the day of the next day. Not only were the patients happy but other staff members were too since they weren’t forced to take a day off as well,” Clarke says.
Tooth decay is one of the most common chronic childhood conditions in the U.S., according to the Centers for Disease Control and Prevention, with about one in five children ages 5-11 having at least one untreated decayed tooth. As such, hygienists are focusing efforts on working within school settings to treat children. According to a 2018 report from the ADHA, a school-based program in South Carolina brings hygienists directly to low-income students in 467 schools in 46 districts. And a program in Michigan called Smiles on Wheels, which is run by three dental hygienists, applied more than 1,360 sealants to children in schools in a one-year period.
“The fact of the matter is most children in the United States are eligible for coverage, either through private pay or through a state-funded program, but just because they’re eligible doesn’t mean that they necessarily get the care,” Lynch says. “So by enabling and permitting dental hygienists to directly access patients, that can often be helpful in helping to ensure that that access is in fact available.”
Up next: Pushback from dentists
Pushback from dentists
While direct access has a come a long way in the last decade, there’s still work to be done. Several of the states that don’t allow direct access, including Louisiana, Mississippi and Alabama, are in the Deep South.
“The holdup is largely antiquated state laws that need to be changed,” Lynch says.
Safety, in particular, has been a long-time concern about direct access, Aberle says.
“For a long time the fear was that it’s not as safe since dentists go to school for four years post-college and some hygienists have programs that are two or three years out of high school, so people’s concern was that hygienists may not know all of the medical complications,” Aberle says.
More from the author: The states with the best and worst oral health in 2018
“But we use Colorado a lot as an example. We have hygienists who have owned their own practices since the early ‘80s and our board doesn’t see an overwhelming number of hygienists who are having malpractice cases, and the ones who have had malpractices cases, a lot of them worked in traditional dental offices. The ones who are practicing by themselves are usually very up to date on standards and taking a lot of extra CE courses. This is their business, their livelihood, like just a dentist, so they’re investing a lot into their education and their practice.”
Lynch agrees that lack of education or certification is a common misconception.
“Regardless of where you to go dental hygiene school at, there are national standards in this country, just like there are national standards for dentistry,” she says. “So regardless of which state a hygienist graduates from and ultimately is licensed to practice in, hygienists are educated to deliver all of the services that they’re educated for. If I’m in a state that doesn’t provide for direct access or limits my scope, essentially I’m not being able to practice to the full extent of my education.”
Aberle says she has heard dentists argue that if hygienists open up their own dental hygiene practices, they won’t be able to afford liability insurance. But in a state like Colorado, all hygienists who practice - regardless if it’s in their own practice or in a traditional dental practice - have to have liability insurance, which is roughly $77 per year.
“That shows you that we’re obviously not a super high risk because if we were a super high risk, then insurance companies would be charging us a lot more,” Aberle says. “And if they were getting an overwhelming number of malpractice claims against hygienists, they would either not insure us or they would charge us a lot more.”
A changing business model can also be a source of concern for dentists. If hygienists are able to open up their own dental hygiene practices down the street from dental offices, then what happens if patients decide to go there instead?
“If you have a good relationship between a hygiene practice and a dental practice, it can be a really great referral back and forth,” Aberle explains. “Obviously the hygienists will find problems that need restorative care and they can refer to the dental practices. Likewise, in Colorado a lot of dental practices are having a tough time finding hygienists right now, and so if they could just utilize the hygiene practices that are near them, they wouldn’t have the overhead and additional salary for staff and they could create those good referral relationships.”
Clarke shares a similar sentiment and says the argument regarding dental offices losing patients is actually the opposite.
“EPP hygienists are required to refer patients to a dental office for annual exams and care,” she says. “If an EPP hygienist has already triaged the patient, other dental care can be expedited. Just as general dentists refer to specialists for endo, perio or oral surgery, hygienists must refer to a general dentist for their specialized care.”
The future of dental hygiene
It seems that the dental industry is often playing catch up to the medical industry, and direct access is no exception. The medical industry has diversified its workforce with nurse practitioners and midwives, and Aberle hopes the dental industry will soon follow suit.
“I think dentistry eventually will catch up and say these people are educated and licensed to provide care and it’s within their scope of practice, so they should be able to practice to the fullest extent of their education. I think eventually all the states will have to step into 2018 or 2020 or whenever it happens and just catch up with what’s going on in the medical industry in general,” she says.
Trending research: Study finds more than 60 percent of people suffer from dental fear
Technology, especially teledentistry, is shifting patients’ perceptions of dental care and how they receive treatment. And with more people requesting after-hours or weekend appointments and affordable care, dental hygienists are filling that void.
“I think medicine is kind of opening patients’ eyes to their options with medical care, and so patients will also start asking for those options with dental care,” Aberle says. “The traditional 8-to-5 doesn’t really work for a lot of people anymore, and so you have virtual doctors where you can do a video call. There’s also an app called Toothpic where you can take a photo of your tooth and send it to a dentist and get some advice.
“Obviously there’s part of dentistry that’s still surgical, so you’ll still have to go somewhere and get that taken care of, but I just feel like because technology and the medical industry are evolving, patients will start asking us for those same options in the dental clinics. Eventually we’ll just have to adapt to the changing world.”