The 5 biggest misconceptions about imaging coding and reimbursement
Dental technology and the material sciences are advancing at a rate never before experienced by the dental industry. It is difficult, if not impossible, for the average practitioner to understand and appreciate all the new “stuff” that has been developed and introduced to dentistry over the past 10 years. Things that not too long ago seemed like science fiction have now become reality.
Dental technology and the material sciences are advancing at a rate never before experienced by the dental industry. It is difficult, if not impossible, for the average practitioner to understand and appreciate all the new “stuff” that has been developed and introduced to dentistry over the past 10 years. Things that not too long ago seemed like science fiction have now become reality.
Many of those new technologies, materials and techniques are rapidly becoming commonplace in the average dental practice and most will see widespread use in nearly every dental practice in the very near future. That’s the good news for both our patients and for the doctors who implement these new advances. The bad news: Reimbursement for these new technologies, materials and techniques has not maintained the same pace of advancement.
In fact, the ADA’s Code Maintenance Committee has been challenged to keep up with this trend. In many instances, technology, materials and techniques that were once used and easily described by the CDT code set are now obsolete and have been replaced by newer diagnostic and treatment solutions.The adoption of codes that best describe the service provided is sometimes hindered by the fact that it takes time for dental researchers to provide enough evidence to support the efficacy of the new technology, material or technique for a code to be adopted to describe it. In most cases codes will not be considered for addition to the CDT to describe services where there is insufficient evidence based support for the service.
Trending article: CDT 2016: 6 changes shaping dentistry
In today’s world, the new advancement is introduced to the market before potential insurance reimbursement for that new advancement is ever considered. These are a couple of the reasons why the code committee is struggling to maintain a code set that adequately describes the many new products and procedures used today. If the powers that be are challenged to keep up, how about the practice that is working diligently to code the procedure appropriately? The larger, more daunting question may be: “Now that I’ve bought the newest, latest, and greatest ___, how do I get paid for using it?” Unfortunately, the venders of the technology, product or service may not be providing accurate information to the practice regarding the associated coding of that technology, product or service.
In the case where there is a code that accurately describes the procedure, understand that just because a code exists that describes the procedure, this does not mean that the insurance carrier must reimburse it. The practice must always submit claims for services using the code that best describes what was done and then let the carrier process the claim according to the parameters established in the plan. If there is no code that currently exists to describe the service, the non-specified codes (DX999) should be used.
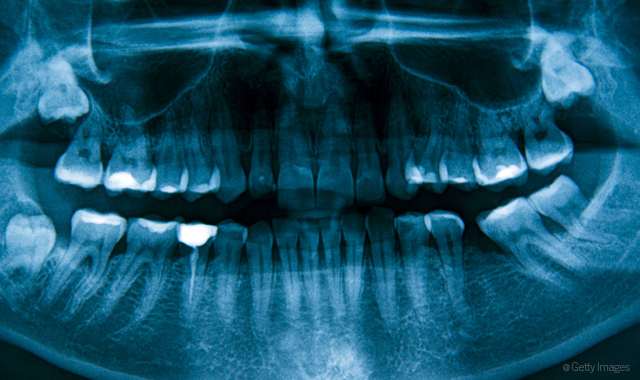
So, specifically, how does all this affect dental images? Continue to page two to read about the five biggest image misconceptions.
Standards are met by producing an image
Before a claim is sent, the following criterion should be met and documented in the clinical record to support the claim submitted to the carrier:
- The doctor must assess the patient and order the image be taken based on medical necessity (not just because the patient’s insurance will pay for the image
- The image must be taken and the resulting image must be of diagnostic quality
- Finally, the doctor must assess the radiographic and note the findings
Trending article: The top 10 things you need to know about ICD-10
Size doesn’t matter
With the advent of the digital radiographic revolution, the images produced are not limited by the film size. In the past, radiographic films were produced in uniform sizes. Today, with the advent of digital images and the software that can help produce the images, the image produced may not be of a conventional size. Take for example the elongated BW images that can be produced by some of the technologies. The BW codes are specific about number and silent about the size of the image generated. In our example of the elongated BWs generated by some of the newer technologies, two images are produced, one for the right and one for the left. Although these elongated images generally contain the same information that four conventional bitewings contain, only two were taken. These images would be submitted as two bitewings, not four bitewings.
Continue to page three for more...
All images are the same
The technology used to capture the image matters: CBCT services are viewed differently from conventional dental radiographic images. The reimbursement for CBCT is not based on the image(s) produced using CBCT. The reimbursement for CBCT is based on two variables:
- The area involved in the capture of data
- The interpretation of the image.
This system more closely mirrors the billing/coding system seen in medicine where a facility captures the image and a radiologist interprets the image. So, if CBCT technology is used to capture data associated with a “field of view of both jaws; with or without cranium,” any subsequent images produced from this capture would be included in this “pack” of data captured, 2D or 3D. Additionally, the multiple images that can be produced from the pack of data should not be billed separately. The billing of multiple individual images produced from the pack of data including a “field of view of both jaws; with or without cranium” could be consider unbundling and potentially problematic. The best code(s) used to describe the use of CBCT technology are the CBCT codes, not the conventional 2D radiographic image codes.
Trending article: SNODENT and the future of dental EHR coding
Looking at the interpretation variable associated with CBCT technology, codes were developed to describe situations where the CBCT information was either:
- Captured (not interpreted) by a provider
- Captured and interpreted by a provider
- Instances where the information is only interpreted by a provider
(The submission for reimbursement of the interpretation of the image has also been limited to “a practitioner not associated with capture of the image” and the individual who only interprets the image must produce a “report” of their findings). This means that multiple dentists practicing in the same location or other dentists who have ownership of the CBCT machine may not bill for an additional interpretation of the CBCT.
Continue to page four for more...
The use of new technology will yield higher reimbursement
Existing standards of care ultimately dictate what the carriers consider for reimbursement and frankly should help guide the dentist in making diagnostic and treatment decisions. In today’s world, standards of care are established by evidence-based review and like the technology we use, are evolving.
The more we know (by testing and outcomes), the more dental standards are changing. Relating this to the dental imaging world (based on the prevailing standards of care) should every patient be exposed to a CBCT? The answer is no, unless that patient is having implants placed, wisdom teeth removed or some other service where the standard establishes a CBCT review should be conducted before proceeding with treatment.
Trending article: Exploring average patient cost per practice
Should that scan be needed to provide the prevailing standard of care in anticipation of a “qualified” treatment, yes. To take a CBCT on a patient that does not have a condition where the standard requires a CBCT could be considered overkill, medically unnecessary, and would not be considered for reimbursement by the patient’s insurance carrier and potentially problematic.
Many carriers will reimburse CBCT technology when the claim is supported with information that establishes the medical necessity (prior to implants if implants are covered by the plan or oral surgery that could damage surrounding structures). CBCT technology will not be considered for reimbursement in situations where the CBCT is deemed medically unnecessary based on prevailing standards of care. Bottom line, the practice should not use CBCT technology to generate a PA.
Continue to page five for more...
If the insurance pays, the billing/coding was done properly
Most claims for images 2D, 3D or photographic are auto adjudicated. This means that if the claim for an image is submitted to a carrier and that claim meets the criterion established in the plan (subject to the established plan exclusions and limitations) it will be processed without review and paid with no other information needed. This can be wonderful if the claim is accurate but dangerous if the coding/billing is misunderstood and results in a payment that is not justified. It will be extremely important in the event of insurance audit or professional review that the doctor ordered the image based on medical necessity, that the doctor reviewed the image and that it was billed correctly. Otherwise, there could be a problem.
Trending article: Dental benefits: Use them or lose them
The bottom line
The doctor is ultimately responsible for insuring that the billing/coding for that new technology, service or product is done correctly. The claim must be accurate and the information recorded in the clinical record must both establish and support the medical necessity for the service provided. Additionally, the information on the claim form must be accurate and the service provided described on the claim form using the current code that most accurately describes the service. Understand the misconceptions and you will maximize the legitimate reimbursement while reducing the risks associated with reimbursement any new technology, product or service.
Product Bites – January 19, 2024
January 19th 2024Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Adravision, Formlabs, Owandy Radiology, Henry Schein Orthodontics, Dental Creations, and Dental Blue Box. [5 Minutes]
Product Bites – January 12, 2024
January 12th 2024The weekly new products podcast from Dental Products Report is back. With a quick look at all of the newest dental product launches, Product Bites makes sure you don't miss the next innovation for your practice. This week's Product Bites podcast features new launches from Videa Health and DentalXChange.